how to better share the contraceptive burden
understanding male contraception
On this page you will find all the information about male contraception.
Do you still have questions? Maxime Labrit answers them !
Free, no information required to connect!
You can connect to the spermanence whenever you want between 7 and 8:30 pm every Tuesday to ask your questions, give your feelings or simply talk about contraception with the designer of the ring.
Male contraceptive methods
Methods you can use today :
Tomorrow's methods :
Contraceptive equity,
a taboo subject.
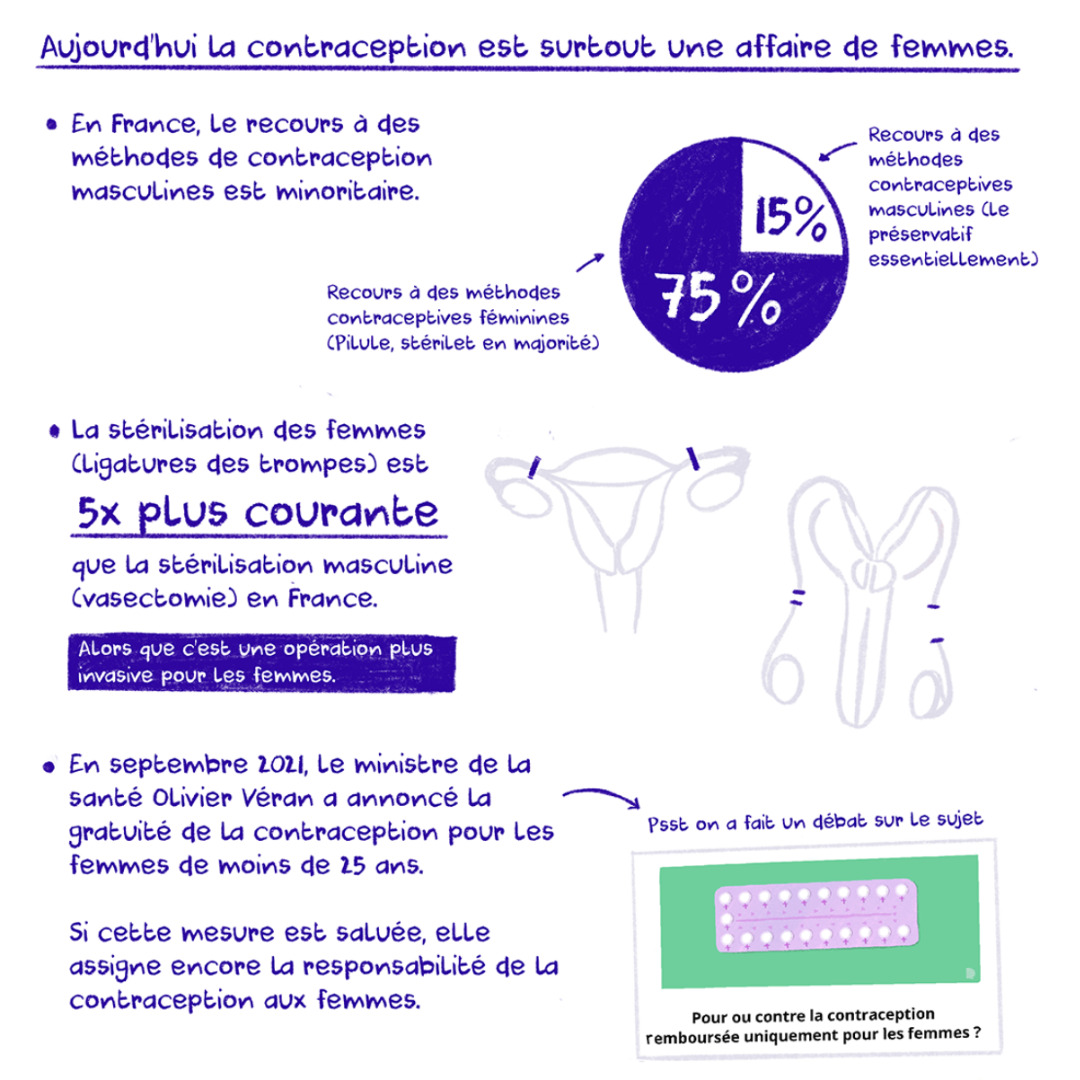
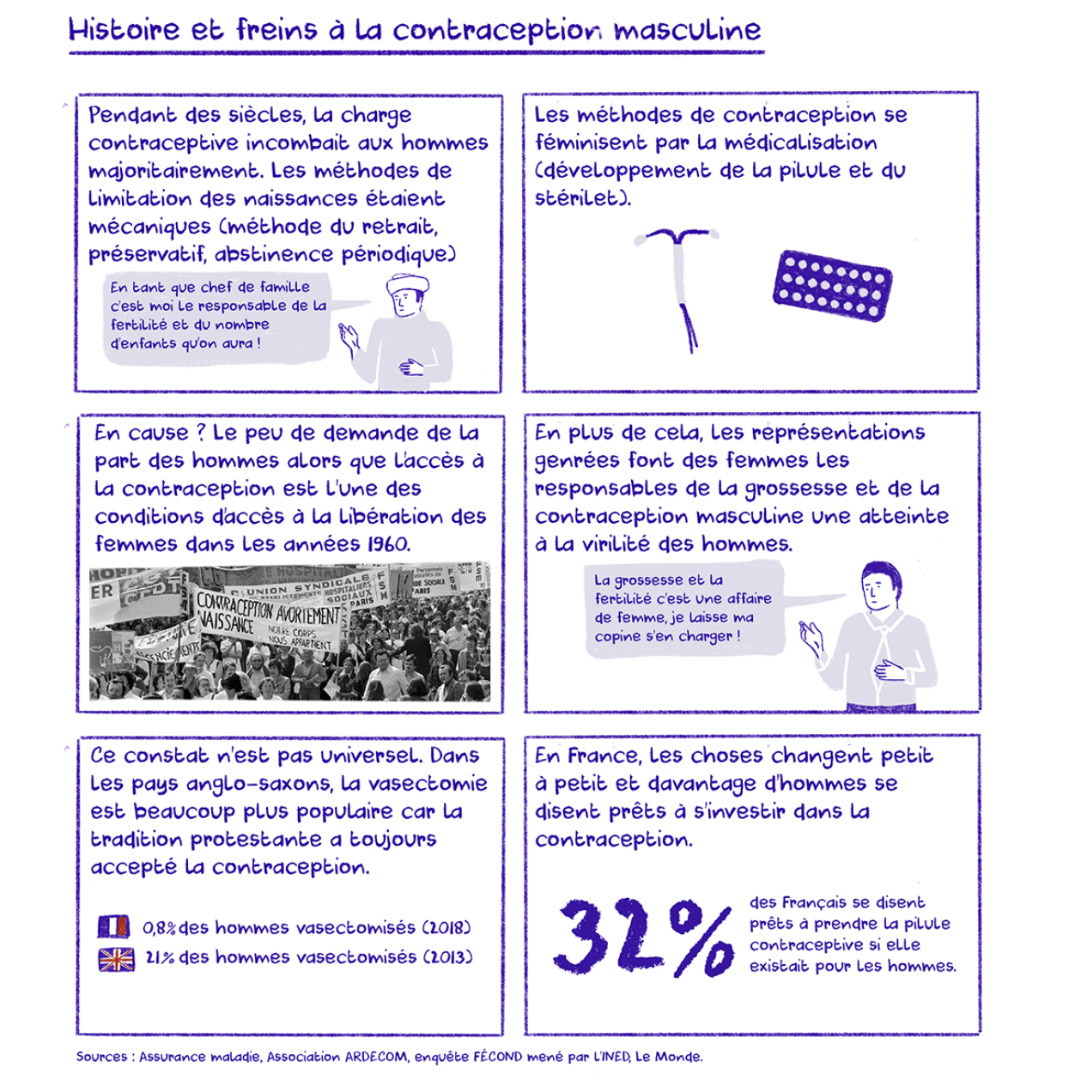
In France, contraception in couples currently relies solely on women in 2/3 of cases (Le Guen et al 2017). Some women find it hard to cope with their contraceptive methods, others remark on the mental load concerning the lack of choice women have regarding contraception. It is high time this changed!
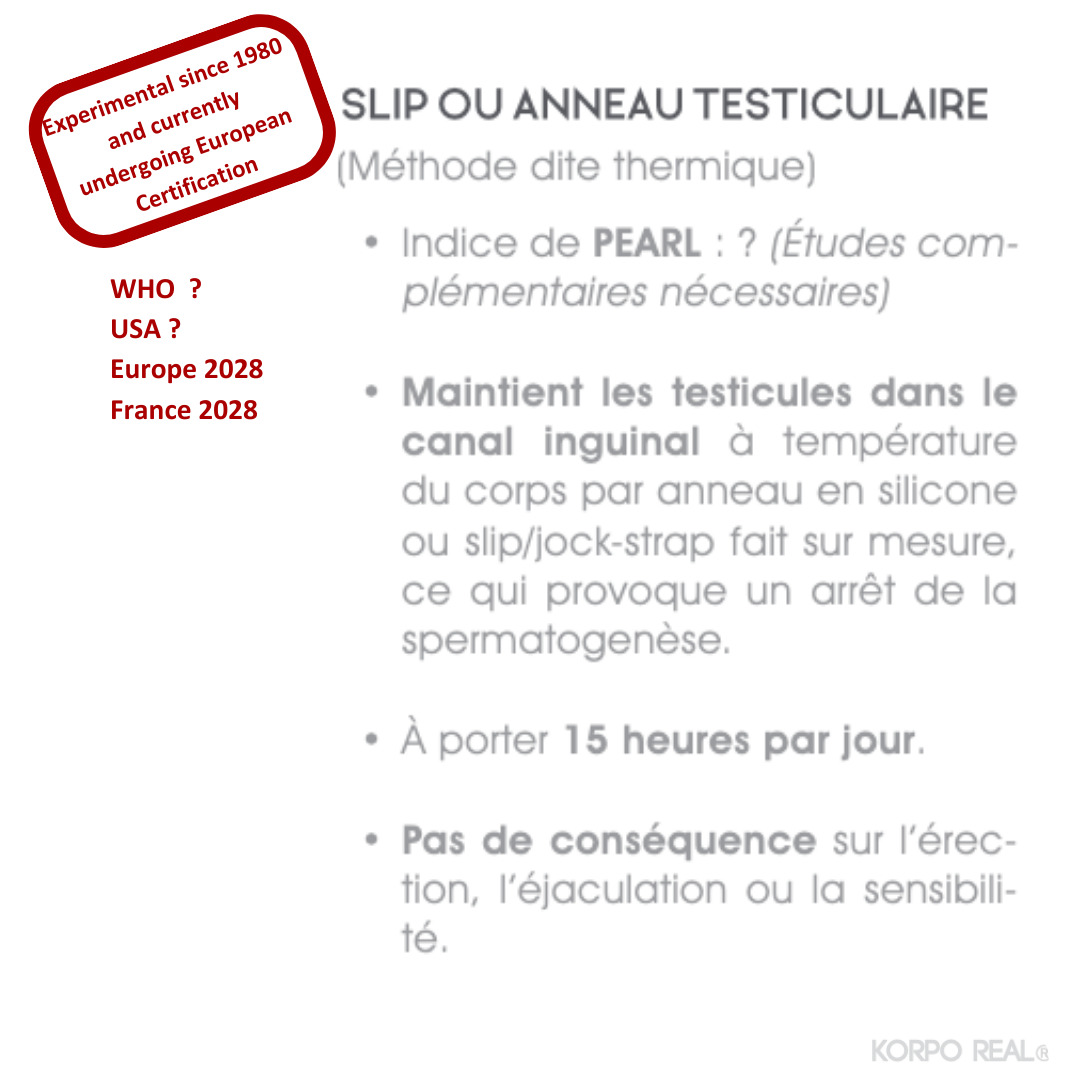
In 2022, it is still not officially possible for men to use the male thermal contraceptive method through testicular lifting, even though it is natural, safe, effective and reversible. However, both internationally and in France, a majority of people are ready to use a male contraceptive method (Heinemann et al. 2005).
Methods exist and are reliable, but their distribution is limited for two major reasons:
- A general lack of knowledge
- Lack of training of the medical population involved in contraceptive prescribing (Mieusset et al. 2022 - Travers and Wanda 2022).
Male thermal contraception.
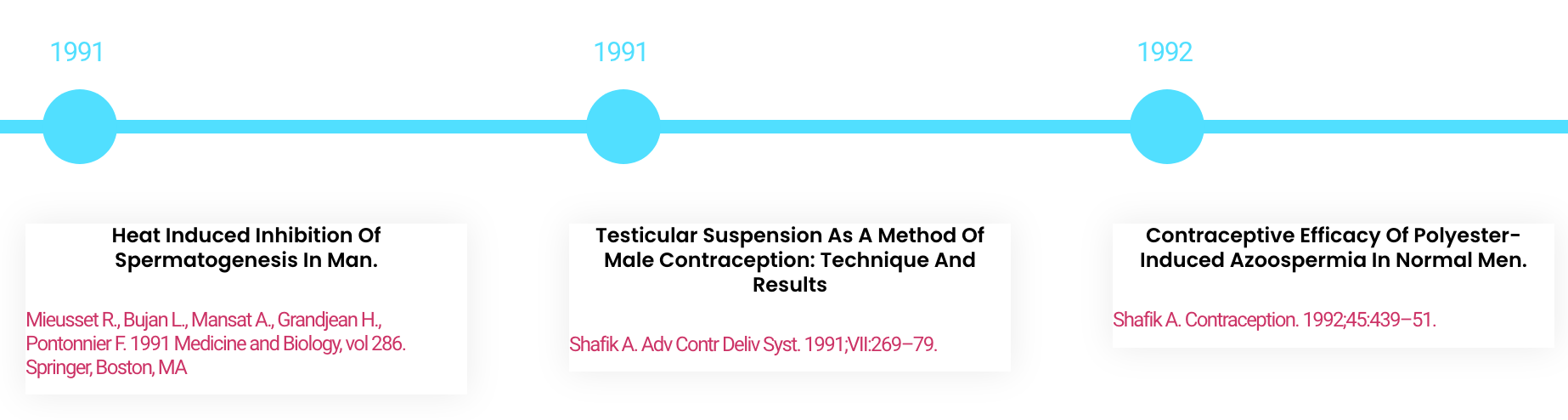
Since the 1990s, the thermal method has been available.
It is based on the temperature dependence of spermatogenesis. It has been clinically demonstrated that the thermal contraceptive method meets the criteria of official contraceptive methods: effectiveness, reversibility, absence of side effects and acceptability. Environmental, social and economic criteria are also important in the choice of contraceptive modalities. See the studies
Thermal male contraception is one of the accessible alternatives, so that men can shoulder their part of contraceptive responsibility in a shared and mutual way. This approach makes it possible to finally address these issues relating to sexuality, fatherhood and fertility.
State of affairs
In 2023, the safe, effective and reversible thermal contraception method is still not officially available.
1979
Creation of ARDECOM (association for the research and development of male contraception)
A group of libertarians set up ARDECOM, which for the next ten years attracted around 200 members to its men's discussion groups.
At the same time in Germany, the Zuricher Hodenbader collective was formed. They explored the same methods of contraception, one of which involved a heated chair:

@dermuger.blogspot 1980 Züricher Hodenbader collective
1985
Dr Roger Mieusset highlights the possibility of contraception by testicular ascent
As part of experiments carried out in conjunction with ARDECOM, Dr Roger Mieusset carried out a study highlighting the impact of testicular lift on male fertility.
A dozen trials were carried out, but the AIDS crisis and other factors put an end to the movement and research.
The wave of AIDS and other factors led to the disappearance of ARDECOM and the Zuricher Hodenbader collective.
2012 - Publication of the book "Contraception masculine" by two doctors to encourage the medical profession to practice the methods and offer them to their patients.
2015 - Ardecom is reformed, some actors like thomas boulou, spermapause appear :


2017 - Maxime Labrit invents the Andro-Switch and the thoreme website to guarantee everyone comprehensive information and a device adapted to the practice. Tens of thousands of users start using testicular contraception in just a few years.
2021 December - The authorities suspend the sale and distribution of Andro-switch until it complies with European regulations. At the same time, they acknowledge the existence of these practices and their benefits in terms of public health.
2022 January
LSF artist supports free access to contraception
To show their support for the cause, LSF designs decorative objects: the REVERSIBLE TALISMANS.
2022 April
Creation of the Entrelac.coop cooperative
A small team decided to set up a cooperative bringing together all interested parties to support Andro-switch in its regulatory and marketing activities. This is the only way of guaranteeing a secure, non-discriminatory supply to all.
2022 May
Direct action by the Slowco movement to raise awareness during the ICMC congress
Petition: For contraceptive equity, now! Launched by the activist media Slowcontraception , over 20,000 signatories, SIGN HERE
2022 September
Entrelac calls for members. 250 people responded, including many doctors
Join the members' team on their website: ENTRELAC.COOP
Libération launched its petition and gathered 30,000 signatories.
2023 March
Entrelac wins the $300,000 Male Contraceptive Initiative MCI Award 2023.
2023 June
Entrelac wins first prize for its practical guide to male thermal contraception, and Thoreme takes second prize for its DIY Andro-swatch applied design research in the International Innovation Prize of the UNESCO Chair in Sexual and Reproductive Health.

2023 September
Internationalization of research. One trial is nearing completion at the CHU de St Pierre in Brussels, involving around 100 volunteers. Another is starting at the HUG in Geneva on 35 volunteers.

2023 October
Installation of the Thoreme micro-industry low-tech module for the manufacture of future certified Andro-switches.
2024 Spring
Pre-clinical testing of Andro-switch followed by launch of safety trial.
2024 Winter
Numerous publications in international scientific literature are produced.
2026
Launch of multicenter trial on andro-switch.
2028
Submission of the certification file to the certification body for CE certification within the year.
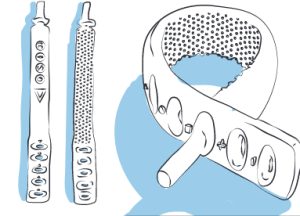
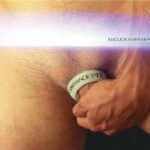
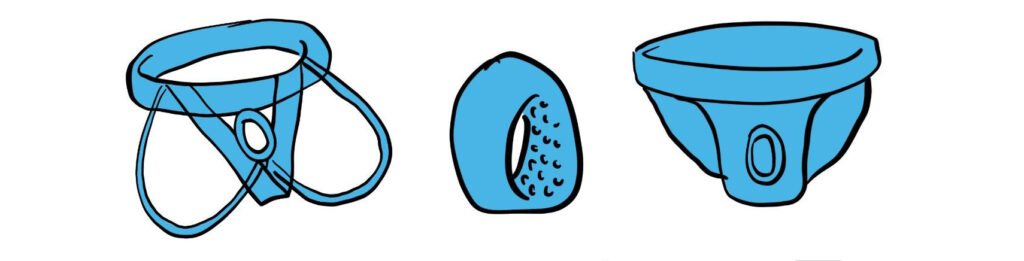
The Andro-Switch ring
The lightest device for male contraception is no longer available for sale pending CE certification.
Support the project by discovering the artist LSF’s reversible talismans!
The Andro-Swatch bracelet
Entirely open source and licensed under Creative Commons, the adjustable do-it-yourself tool is the ultimate applied design research project.
The spermapause or "heated boxer".
As an alternative, if testicular lifting is not an option, these boxer shorts are equipped with a heating element that warms up the testes locally.
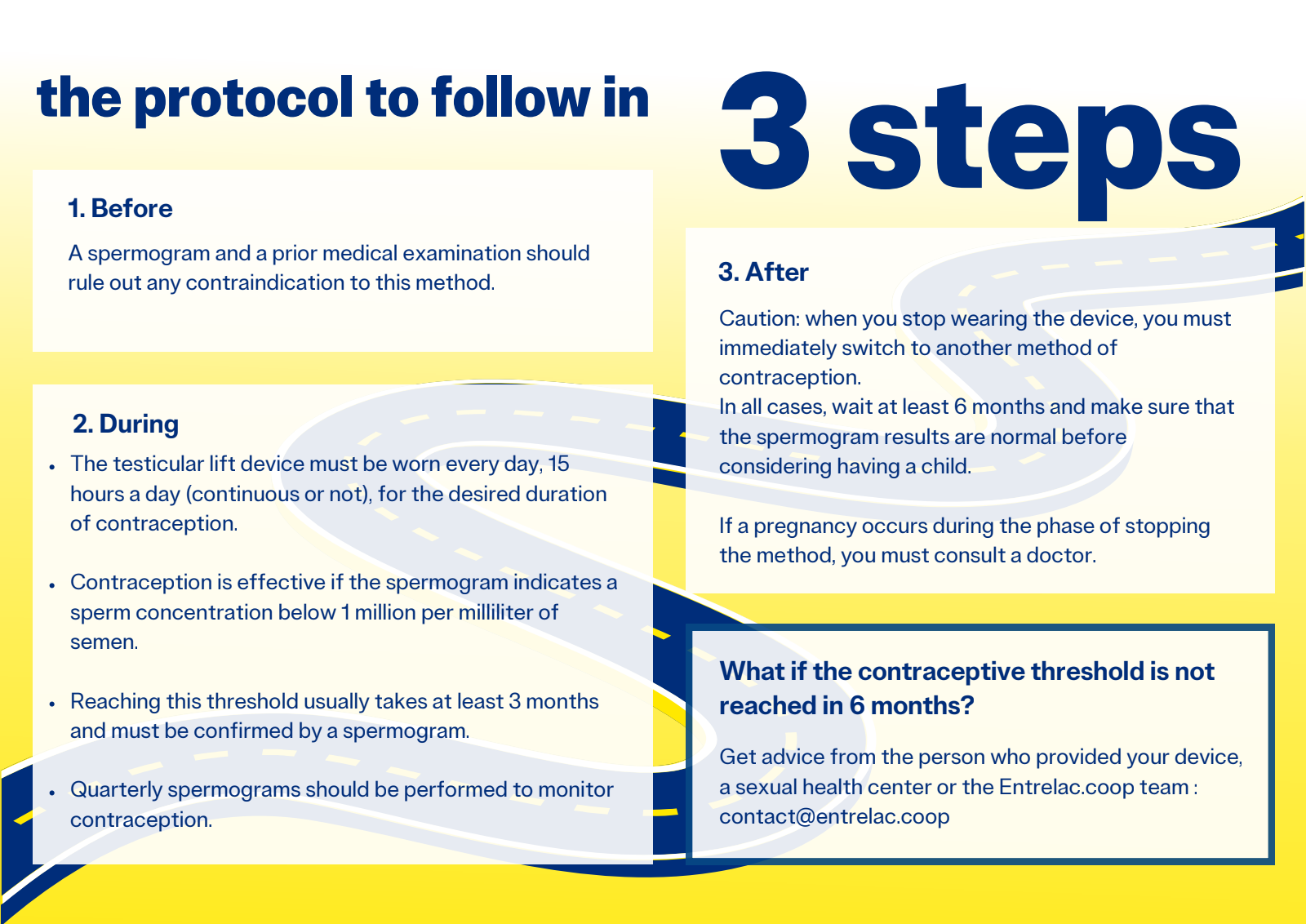
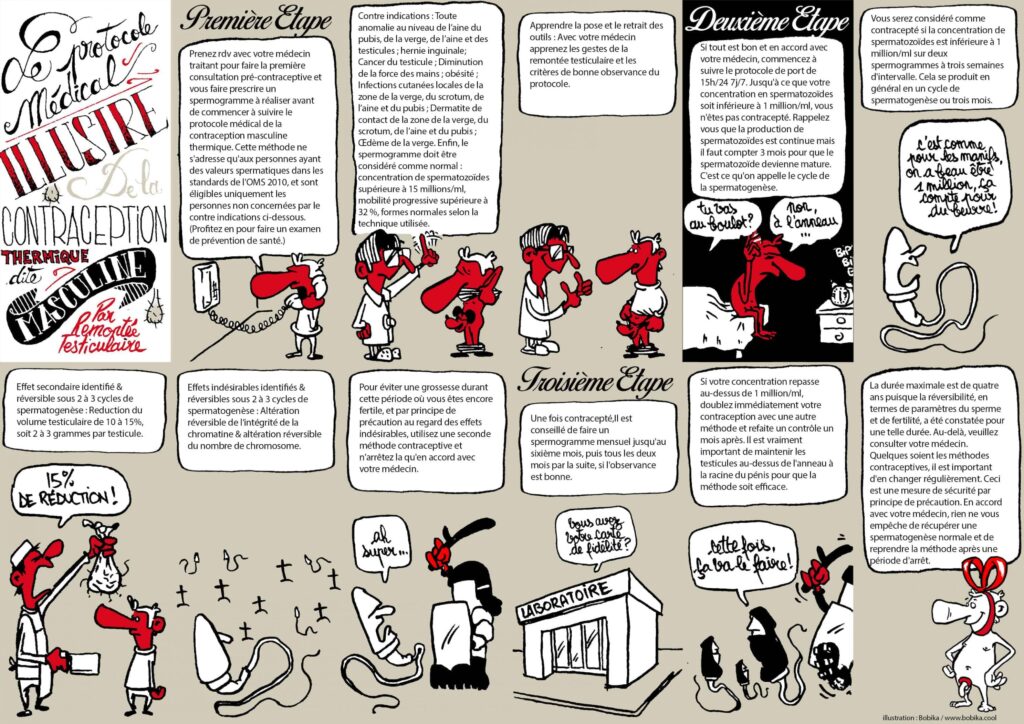
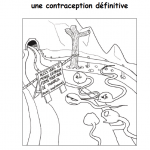
Contraceptive process
In a nutshell:
Check list:
- Make an appointment with your doctor for data collection, testicle examination, and prescription for a sperm test. This website also provides resources for professionals, such as protocols, practical guides, and consent forms. If your doctor refuses, ask for a referral to another professional or contact your local family planning organization for support.
- Contact a nearby laboratory to schedule your spermograms every three months. A map is available in the footer for locations in Europe.
- Choose the device you plan to wear and test it to make sure it is comfortable and effective. Practice using it during daily activities, but avoid wearing it regularly before the first spermogram.
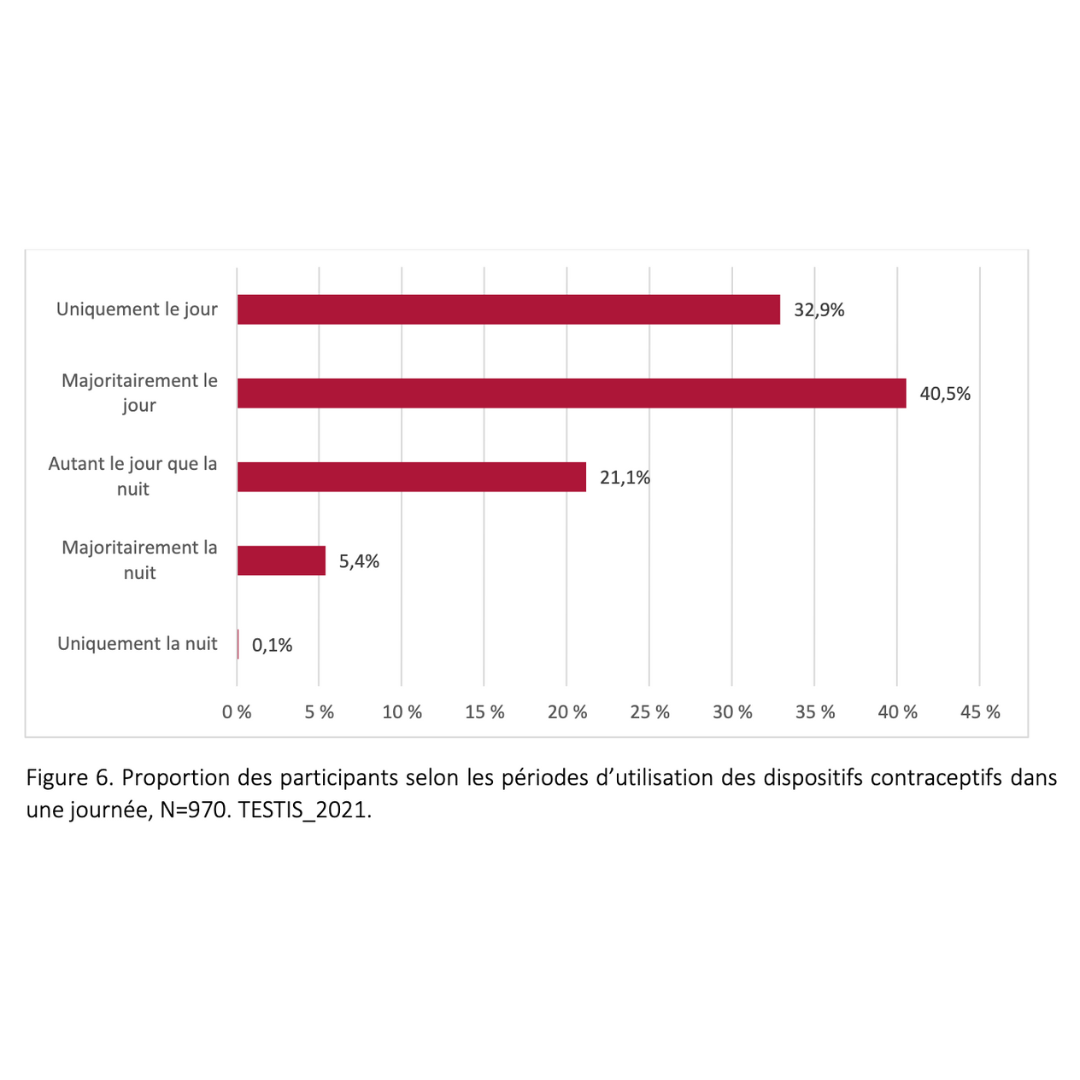
- Plan how you will fit the 15 hours of wear into your daily routine. Think of your day as a 24-hour block, with 14 to 16 hours dedicated to wearing the device. You can wear it during the day or night, continuously or in segments—whatever works best for you.
- People with testicles are currently under-medicalized and people with ovaries over-medicalized in the field of sexual and reproductive health. Use this soft medical follow-up to do some screening and ask for a complete health check-up. This will enable you to do a little screening.
- In France, sperm tests are reimbursed by social security or can be done for around 30 euros. Sperm@home offers an independent monitoring solution, but it does not replace a proper laboratory examination.
- There has been scarce development of male contraceptive methods in the past 40 years. No device to lift your testicles is CE marked yet, meaning they are not officially certified but not necessarily unsafe. Andro-Switch, supported by Entrelac, aims to be the first officially recognized device by 2028. Until then, it is up to each of us to take responsibility.
- The thermal method is unique, with 40 years of practice, tens of thousands of users, and numerous clinical trials and medical theses showing its potential. Remember, you are free to decide what to do with your body, and access to contraception and reproductive health is a fundamental right!
Here to help:
Your attending physician
Family Planning - CeGIDD - CPEF
The thoreme team
Spermanence every Tuesday night
User committees
Social networks
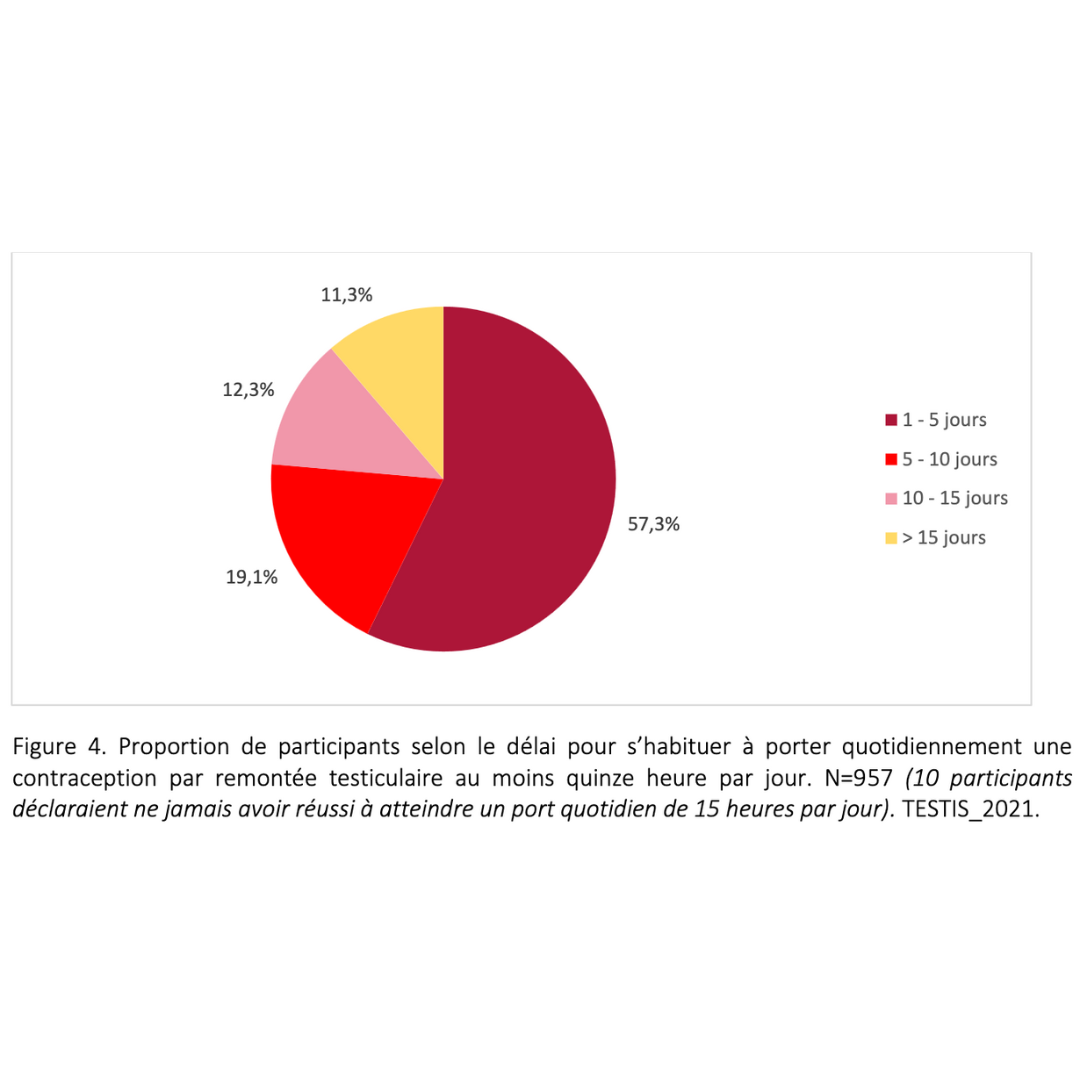
- If you are eligible for the method, you can begin using it. During the first week, gradually increase wearing time until you reach 15 hours per day. If you feel discomfort, remove the device and try again later. Massage the pubic area to relax, and use cream if needed. It may take some time to adjust to this new routine.
- Once comfortable, start wearing the device for 15 hours every day. Until you complete a follow-up spermogram in 3 months, you are not yet on contraception, so use another method alongside. Gradually refine your routine until wearing the device becomes as natural as wearing glasses.
- It is okay if you wear the device for more than 15 hours per day occasionally. It is better to wear it for too long than not long enough.
Need to go faster?
You can schedule a spermogram after two months. You may already be contracepted by then. To speed up the process, increase the frequency of ejaculation to once every two days, similar to post-vasectomy recommendations.
- You can wear the device during the day or night, continuously or in segments. The important thing is to establish a routine that works for you.
- During the initial phase, aim to wear the device for 15 hours a day (between 14 and 16 hours) to determine your sensitivity over the first two to three months.
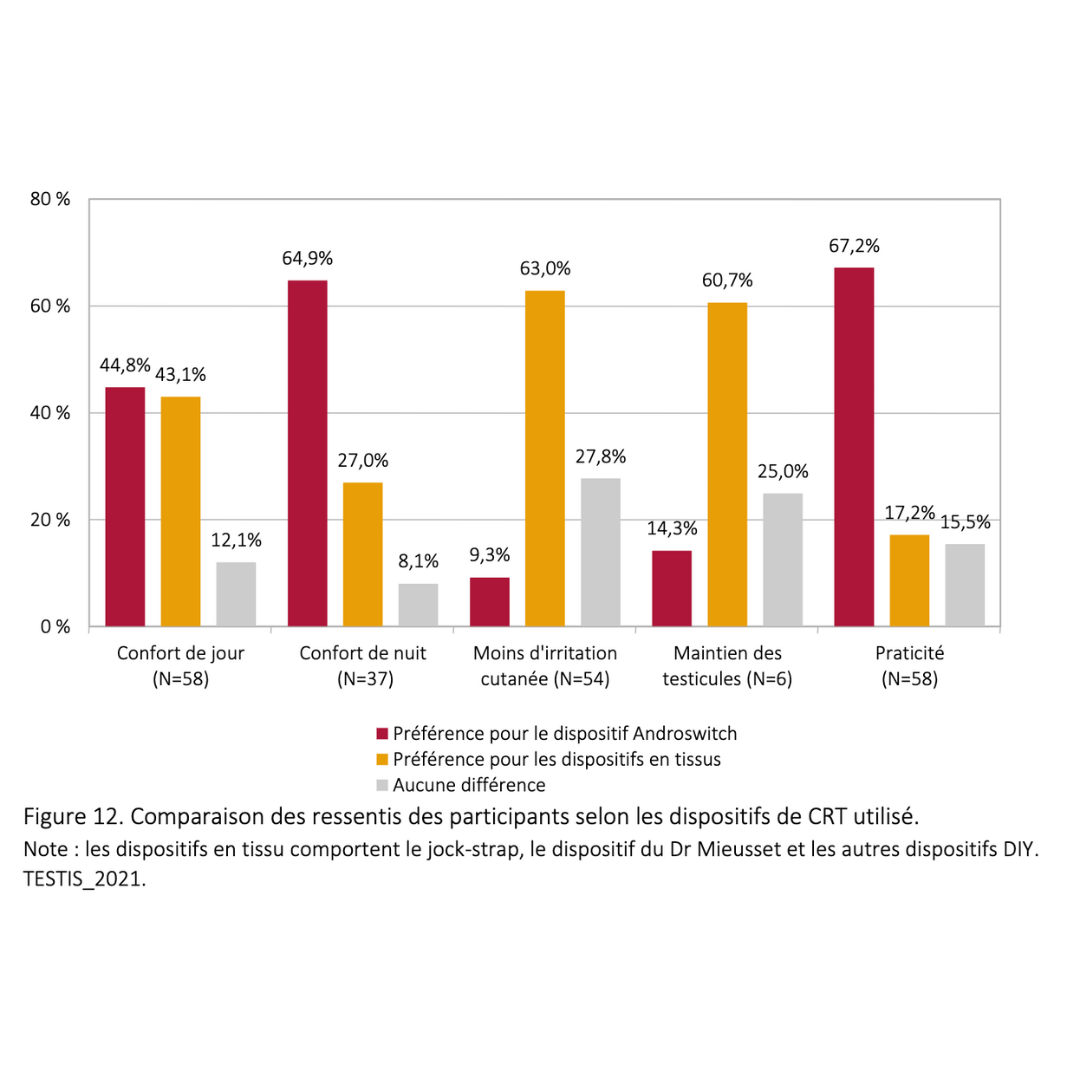
- You can use different tools at different times—such as the ring in the morning and the underwear in the afternoon. The key is to ensure the testicles are elevated for the required 15 hours.
Here to help:
Your attending physician
Family Planning - CeGIDD - CPEF
The thoreme team
Spermanence every Tuesday night
User committees
The entire ring community
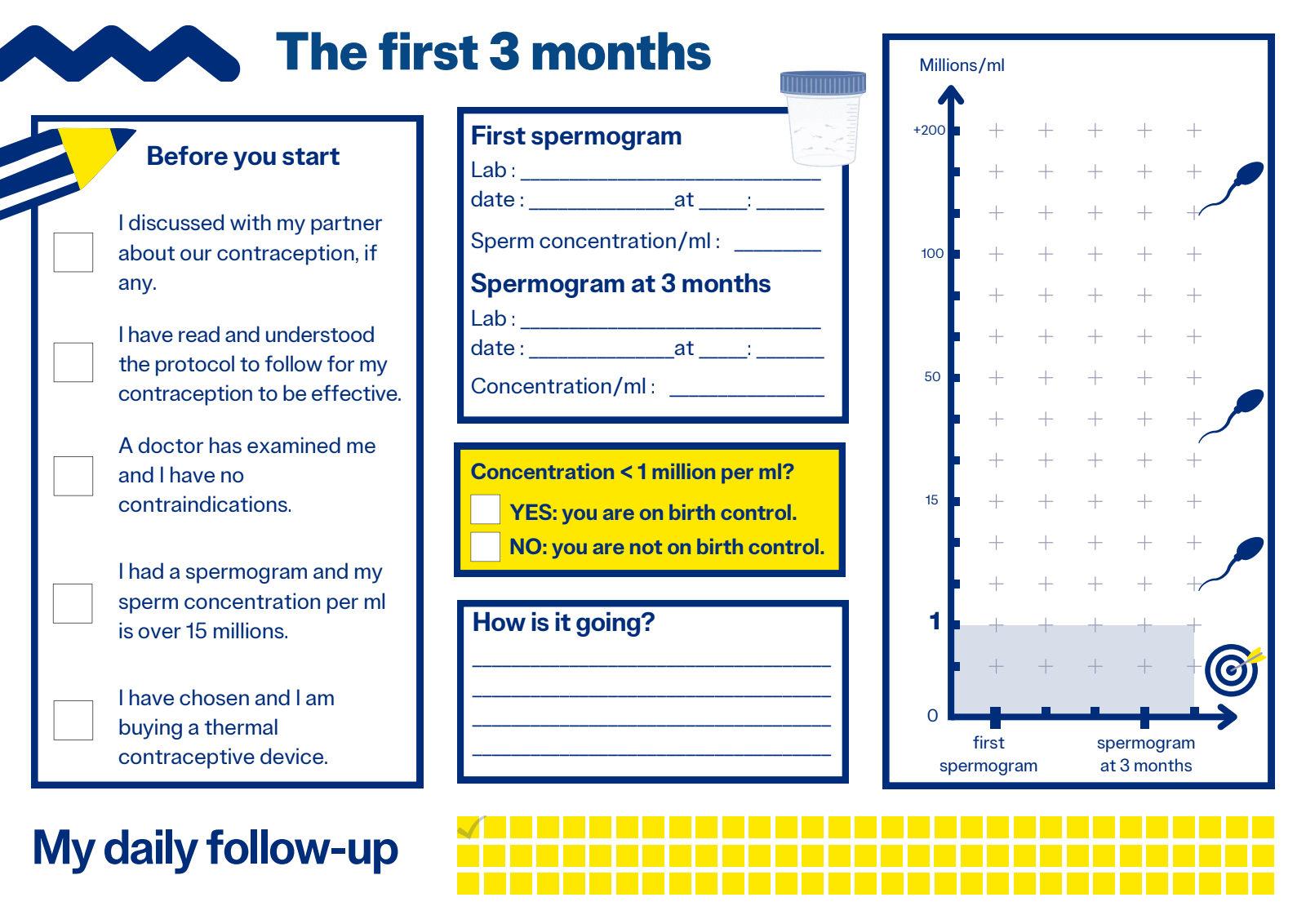
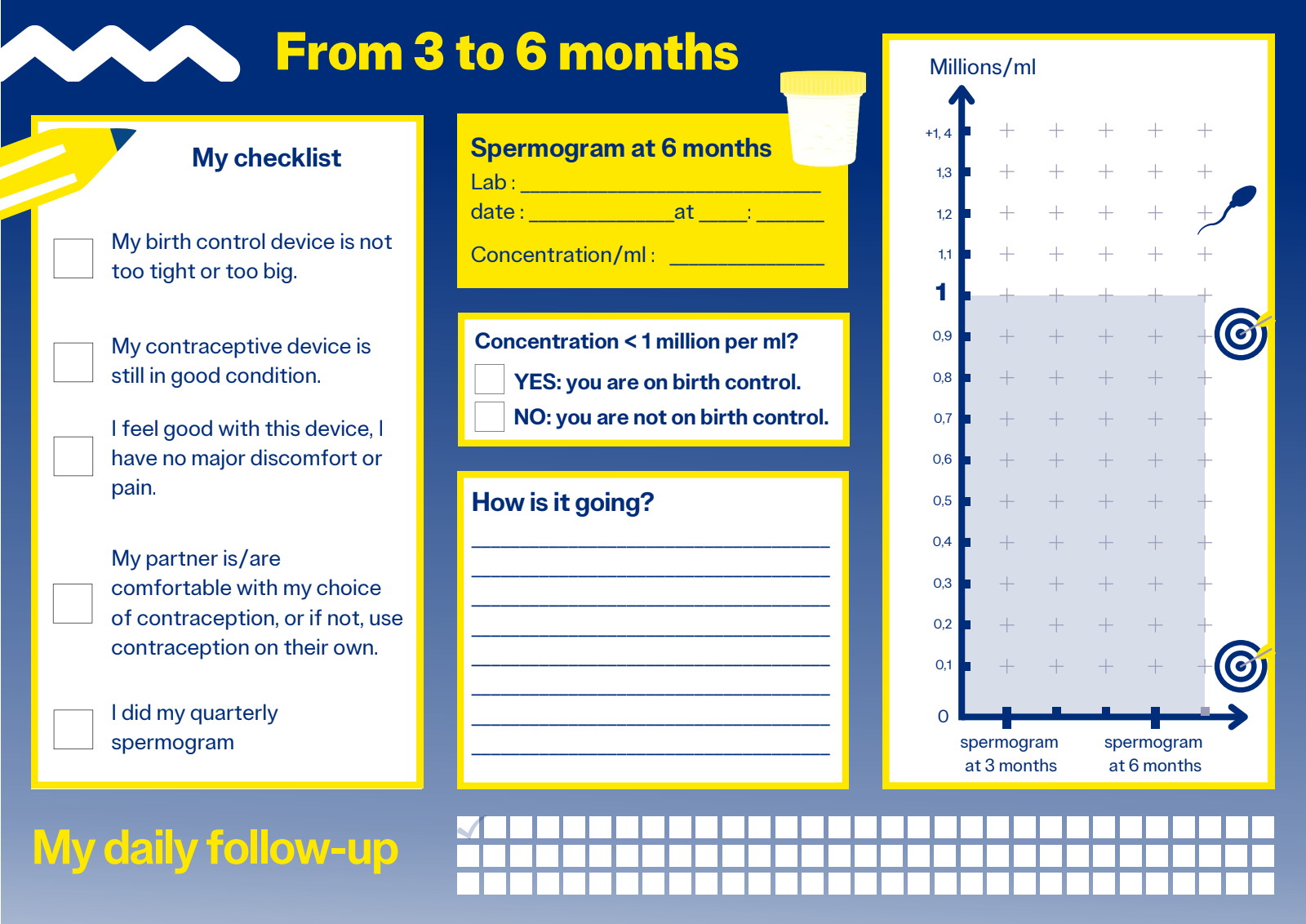
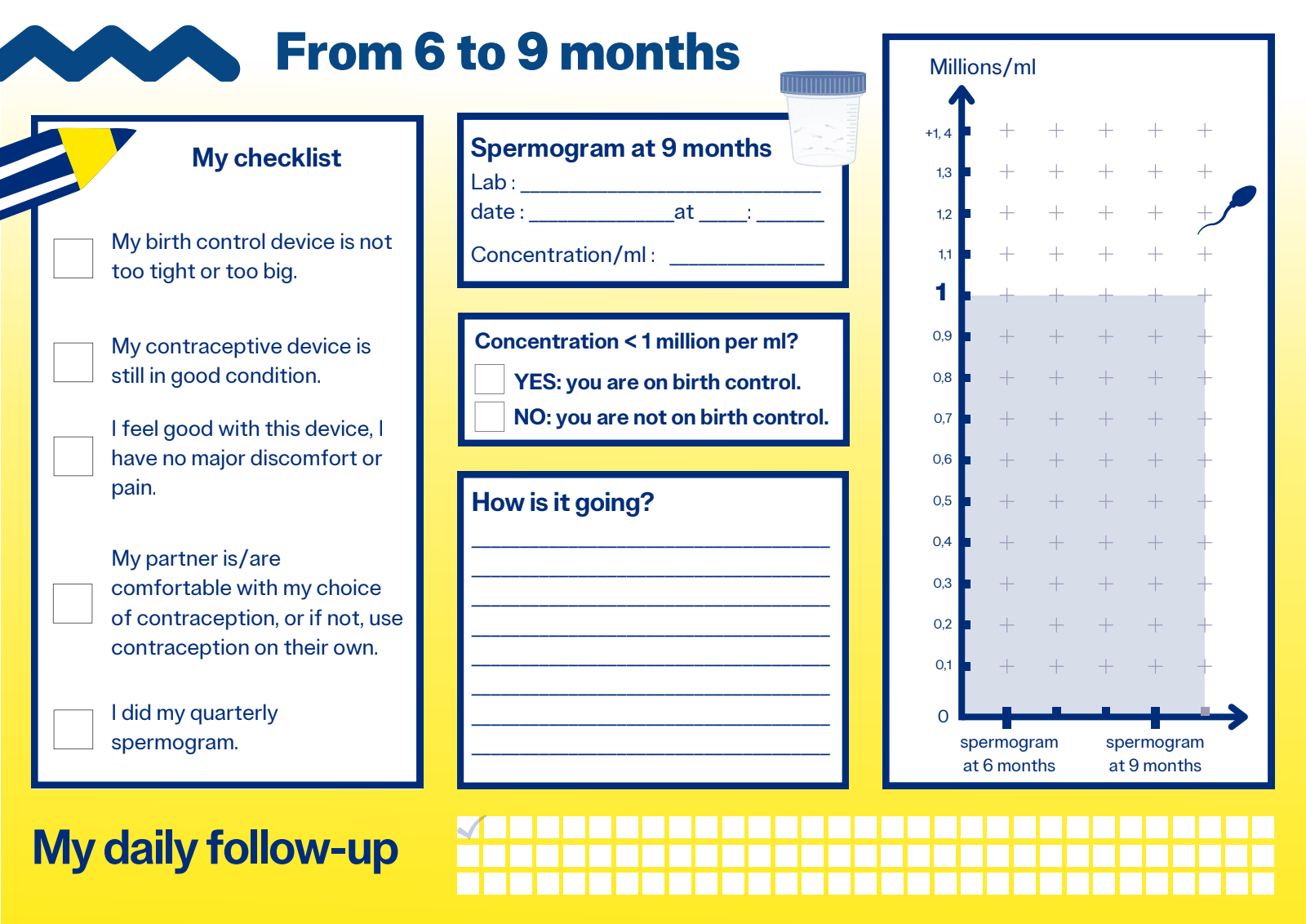
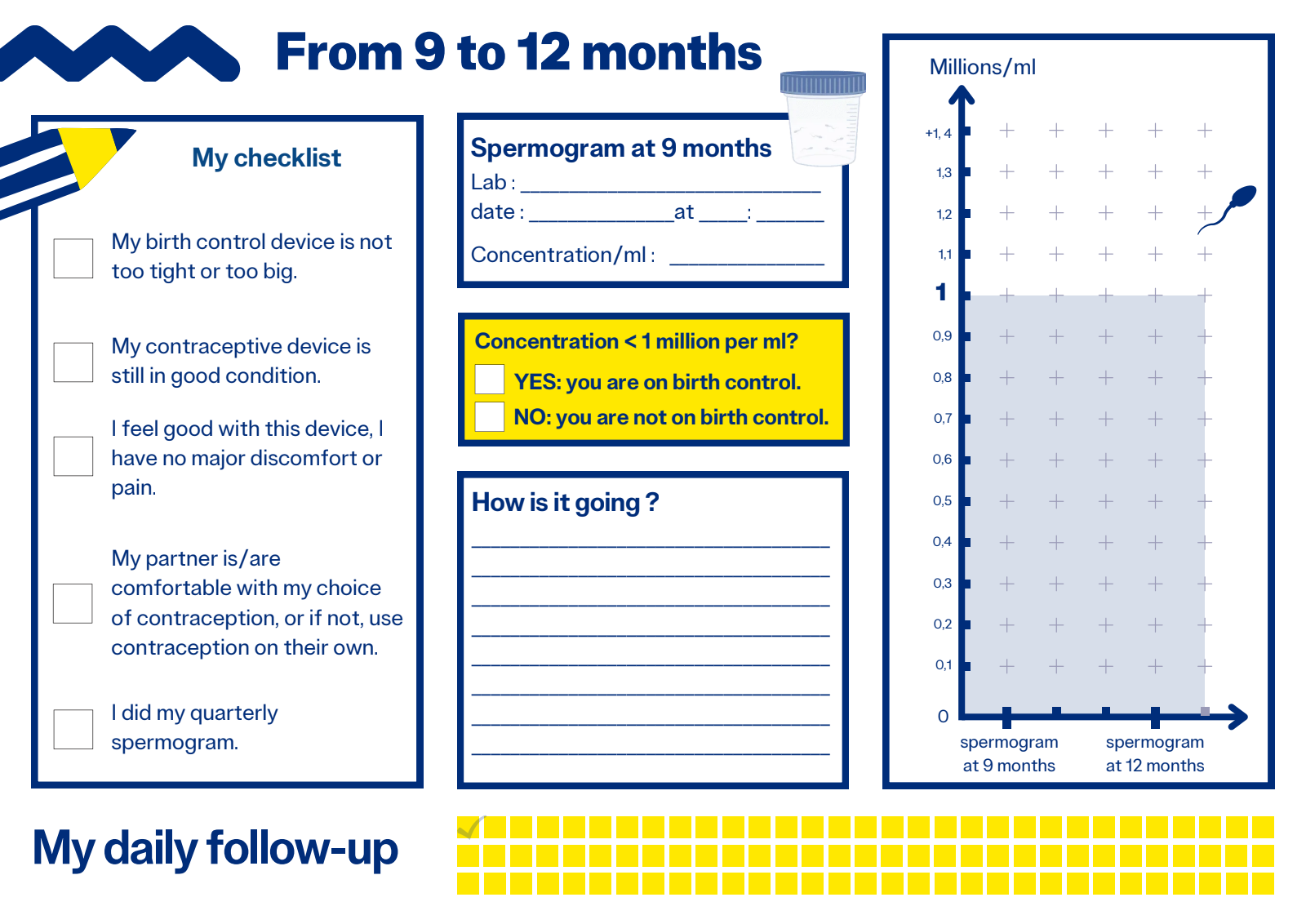
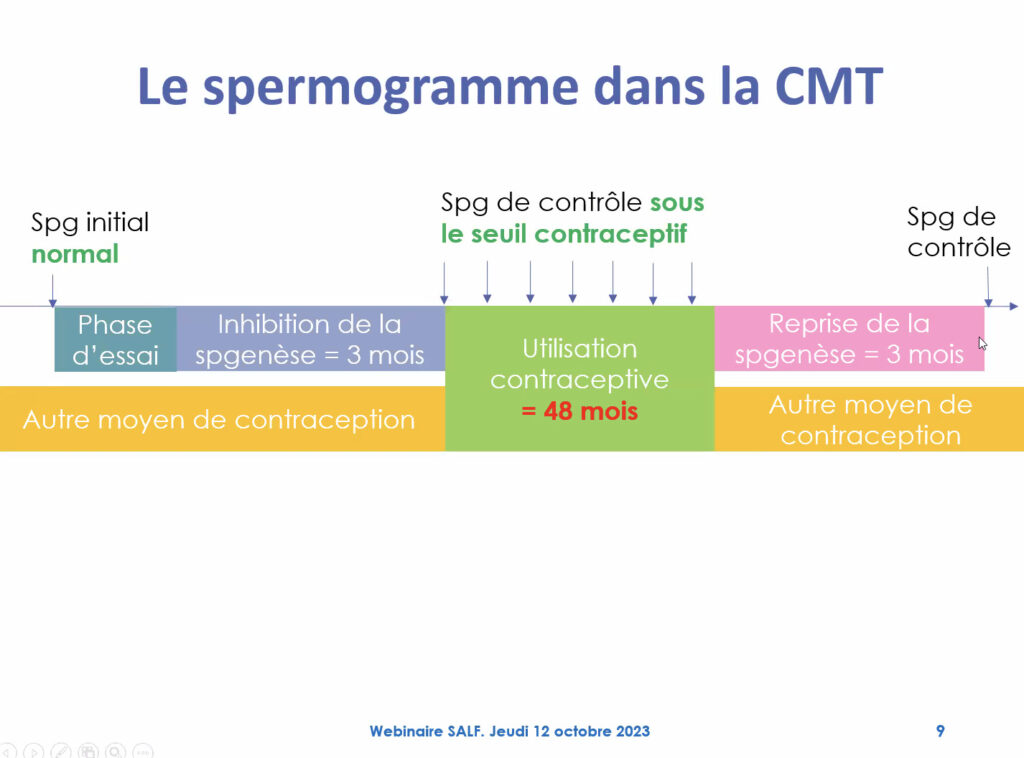
The contraceptive threshold :
Since 2007, the contraceptive threshold has been defined as a sperm concentration of less than 1 million/ml for all mobility types combined. Below this level, you are considered on contraception.
Contraceptive threshold not met:
- If you have not reached the threshold, check if your device is suitable, increase the wear time, and consult a healthcare professional to adjust your approach. Not everyone is equally sensitive to heat; for some, 15 hours is enough, while others may need 17 hours. Schedule a sperm test in 30 days after making these adjustments and continue using another form of contraception in the meantime.
- You can also adjust the type of device, the wear time, and how you distribute it throughout the day. However, in rare cases, this method may not work—sometimes body heat is insufficient or discomfort persists. In such cases, consider switching to another method and contact the Thoreme team for support.
- Once the sperm test confirms a sperm concentration below 1 million/ml, you can use this method alone if you and your partner agree. Continue wearing your device as usual, and perform a sperm test every three months to ensure effectiveness.
- Maximum duration of 4 years
Currently, there are no clinical trials beyond four consecutive years of use. This does not mean extended use is unsafe, just that there is no scientific data yet. After four years, take a 3 to 6-month break before restarting.
Protocols if you forget to wear your ring:
Daily exposure to body heat is crucial. Mistakes happen, and here are some guidelines based on user experience:
Note:
- Long-term use
After using the method for four years, take a 3 to 6-month break, and reassess if it is still suitable. Ask yourself whether this method fits your current goals, including your desire for parenthood. Changing your contraceptive method periodically ensures long-term effectiveness and reduces risks.
If you want to completely stop sperm production, wear the device for an additional one to two hours daily, reducing sperm count to the level of a vasectomy.
If you forget to keep your testicles lifted for more than a day, use another contraceptive method for 30 days and schedule a spermogram at the end of that period.
- In case of unplanned pregnancy
The method has many benefits but also comes with risks. Heat affects spermatogenesis at multiple levels, including genetic changes, which are reversible after stopping use. These changes are similar to those caused by chemotherapy or acne treatments.
Here’s what an embryologist from the Centre de Référence sur les Agents Tératogènes (Crat) and the Académie Nationale de Médecine says about the risk:
"Reading the information on sperm DNA in the context of testicular hyperthermia, the possible risk in case of fertilization with an altered sperm is the development of aneuploidy in the embryo. However, this risk is theoretical, as the likelihood of embryos with chromosomal abnormalities developing is low. Similar risks have not been described in other situations with potential aneuploidies, such as paternal chemotherapy. If fertilization occurs during a period when sperm chromosomes are most affected, there is no need to terminate the pregnancy, as the risks are limited. Prenatal diagnosis for chromosomal abnormalities (blood marker tests and early ultrasound at 12 weeks) is sufficient."
"In reading the elements described on spermatic DNA in the context of testicular hyperthermia, the possible risk in case of fertilization with an aneuploid gamete is that of finding this aneuploidy in the product of conception. However, this is a very theoretical risk since the possibilities of development of eggs carrying chromosomal missegregations are very limited. This has not been described for example in other situations where aneuploidies are possible in spermatozoa (paternal chemotherapy). A priori, in this context, if fertilization takes place during the period when sperm chromosomal changes are most marked, there is no reason to propose termination of pregnancy because the risks are very limited. It is only necessary to consider a prenatal diagnosis specifically designed to detect chromosomal abnormalities in numbers (blood marker assays coupled with an early ultrasound at 12 SA), or even an INFP if the result is positive or doubtful."
Here to help:
Your attending physician
Family Planning - CeGIDD - CPEF
The thoreme team
Spermanence every Tuesday night
User committees
The entire ring community
After stopping, do not plan for pregnancy immediately.
- There could be a risk to fetal development if you don’t wait for your sperm to return to normal after using the method. Use another form of contraception method for a few months after stopping. Allow your body time to eliminate altered sperm—this usually takes 3 to 6 months. Once your sperm count is back within WHO standards, your low-quality sperm is gone, and you can start planning for a pregnancy.
The group of doctors who are members of the Entrelac.coop cooperative will soon be publishing the conclusions of their research on this subject:
2022 - Is there evidence of a link between exposure of pubertal testes to temperatures equivalent to body heat and the risk of testicular cancer? A narrative review.
"Studies on the causes of testicular cancer do not identify heat exposure as a risk factor. Prospective studies on the effects of testicular heat have shown no increase in the risk of testicular cancer."
-> https://drive.google.com/file/d/1p3sDWLgw0TN8doMQ2fIb79JC9U3KpwFj/view?usp=drive_link
Here to help:
Your attending physician
Family Planning - CeGIDD - CPEF
The thoreme team
Spermanence every Tuesday night
User committees
The entire ring community
associations and representatives on the ground
Family Planning, associations and groups offer the public a range of tools for finding out about male contraception about male contraception: experience-sharing, discussion groups, group consultations, workshops, networking.
Movement supported by :
For doctors
Why accompany?
Risk reduction !
Doctors do not prescribe the ring or other devices, but they must provide information on all existing methods, including those currently under development.
If the person freely chooses to use this method, he or she must be informed that it is not yet recognized, and that safety and performance cannot be guaranteed to be equivalent to a certified method.
The conscience clause (at least in France) allows you to refuse to treat a patient, but obliges you to refer the patient to a colleague.
Pre-contraceptive consultation and the prescription of spermograms are part of your role.
At certification
The Andro-swtich ring is currently undergoing certification. Safety testing begins in 2024, with certification scheduled for 2028.
After 40 years of stalemate with pharmaceutical companies unwilling to develop these methods, Entrelac.coop has successfully taken the regulatory steps needed to provide a medico-legal framework for these devices.
A health consent form, a doc'éthique and the Hyppocratic oath are available if you wish.
"I will respect all people, their autonomy and their will, without any discrimination according to their condition or beliefs."
Any doubts about the protocol or the support to be provided?
To benefit from support from one of the doctors in the CMG's "Male Contraception" working group,
write to [email protected] (without patient identification data, as the address is not secure).
Things to look out for with your doctor before starting
Medical history
Testicular descent anomalies (cryptorchidism, ectopia), treated or untreated.
Testicular cancer.
Inguinal hernia treated with mesh.
Testicular torsion treated by fixation of the testicle in the scrotum, preventing ascent;
Abnormal sensitivity of the pubic area, groin, penis, or scrotum.
Poor grip strength.
Severe obesity (BMI ≥ 30).
Testicular examination
Grade 3 varicocele.
Edema of the penis.
Intra-scrotal lump.
Large hydrocele.
Cutaneous filariasis, Elephantiasis;
Local skin infections or contact dermatitis of the penis, scrotum, groin, or pubic area.
Initial fertility evaluation
Spermogram to ensure sperm values meet WHO 2021 standards:
Concentration > 16 million/ml
Total count > 39 million/ml
Progressive mobility > 32%
Normal head shape > 4% (Krüger) or 23% (modified David)
If these standards are not met, try to improve your lifestyle habits (sleep, stress, diet, exercise) and repeat the spermogram after 3 months.
3 key values
1 million/ml :
Concentration below which the risk of pregnancy is greatly reduced.
The contraceptive threshold was defined in 2007:
10 th Summit Meeting Consensus: Recommendations for Regulatory Approval for Hormonal Male Contraception
Journal of Andrology, Vol. 28, No. 3, May/June 2007
Copyright E American Society of Andrology
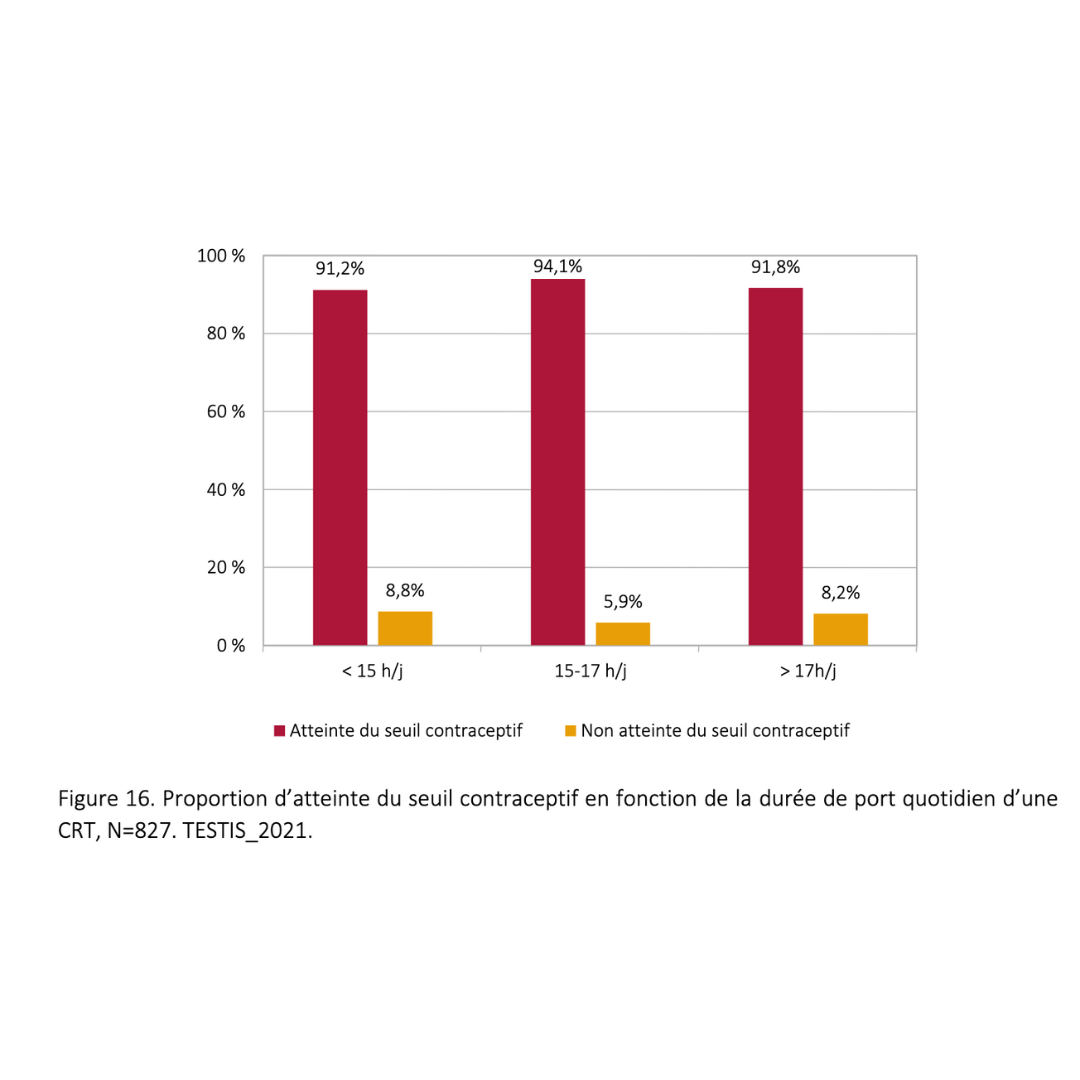
15 hours :
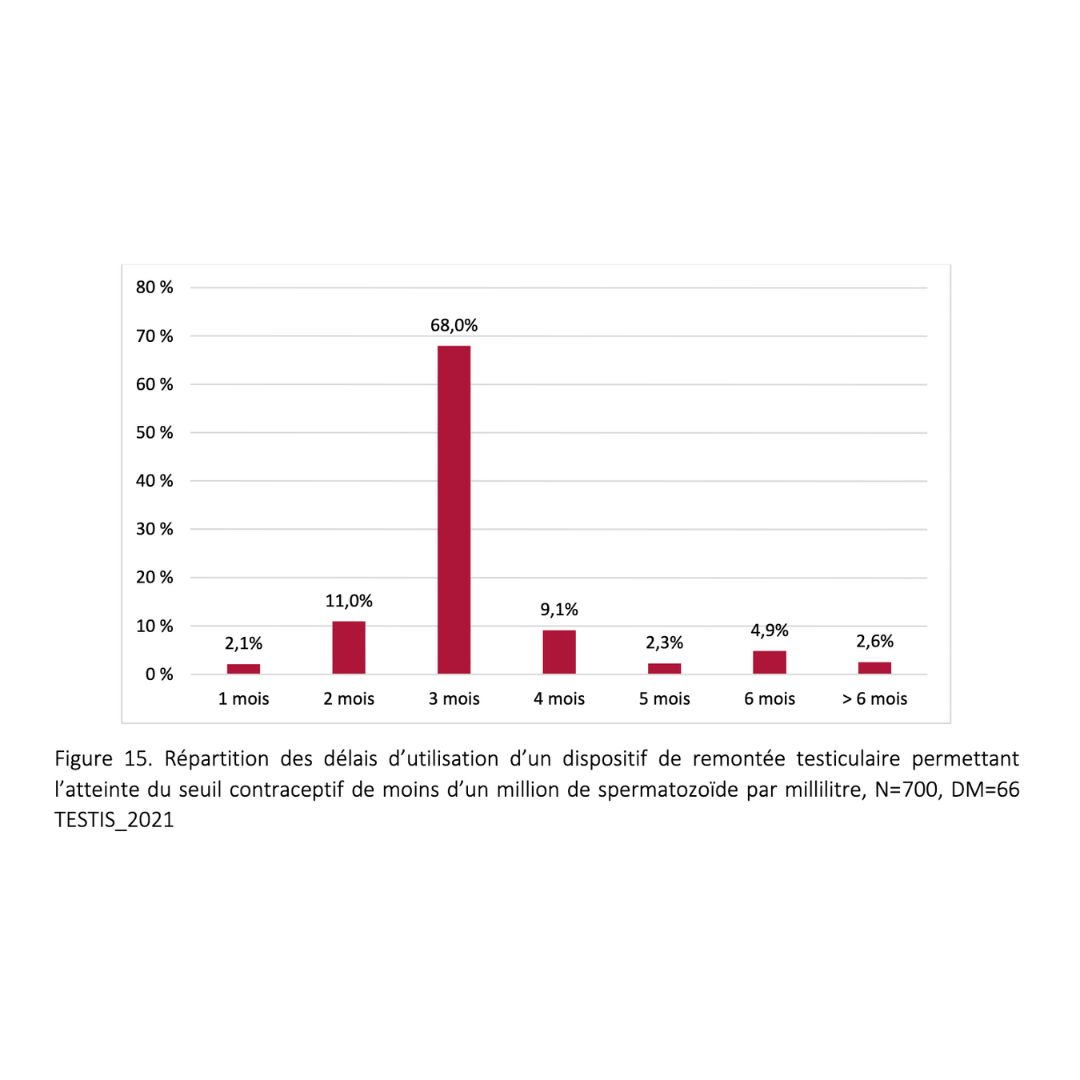
This is the median time between 14 and 16 hours of device use, to ensure that the majority of people reach the contraceptive threshold.
Depending on your individual heat tolerance, you may need to increase the daily wearing time if necessary.
Protocol applicable for 4 consecutive years, renewable after a break of 3 to 6 months.
3 months :
This is the length of the spermatogenesis cycle. Once contraception has been established, checks are carried out every three months.
For the start-up phase, we recommend an initial check-up at two months, with an increase in ejaculations to one every two days. Then one month later, if the contraceptive threshold has not been reached, modify the wearing time and the tool as required.
Around 3% of people are thermo-resistant. If after 6 months of use the threshold has not been reached, suggest other methods of contraception.
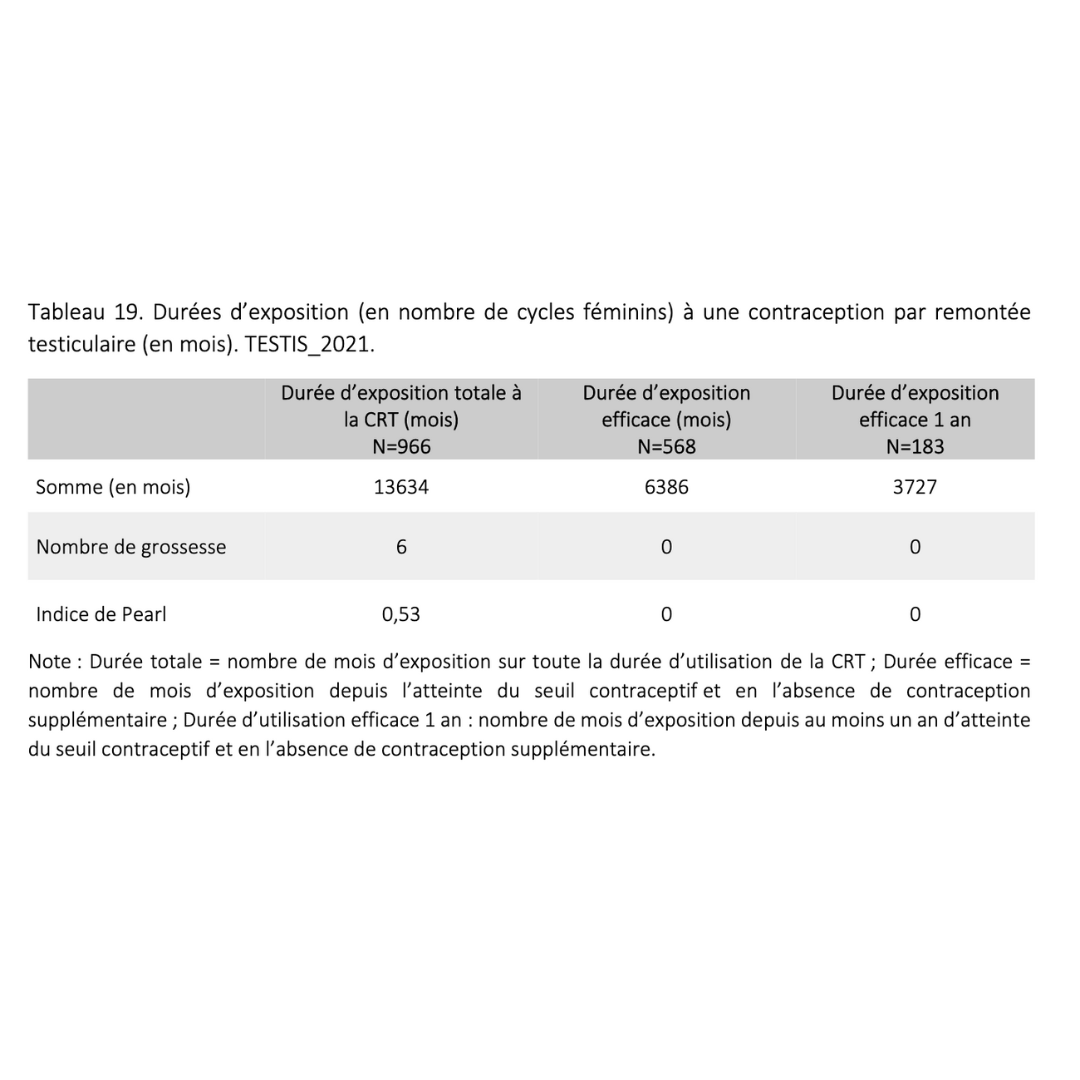
Efficacy: 99.5% - Complete reversibility in 3 to 6 months
Clinical trials
15 tests from 1985 to 2019 :
On cohorts of 10 to 30 volunteers, one over 4 consecutive years.
Followed by over 122 volunteers between 1985 and 2019 for up to 48 months.
Of the 122 volunteers, only one pregnancy was reported due to misuse of the method.
1 unplanned pregnancy out of 1331 exposure cycles.
Excellent reversibility in all tests.
Medical theses
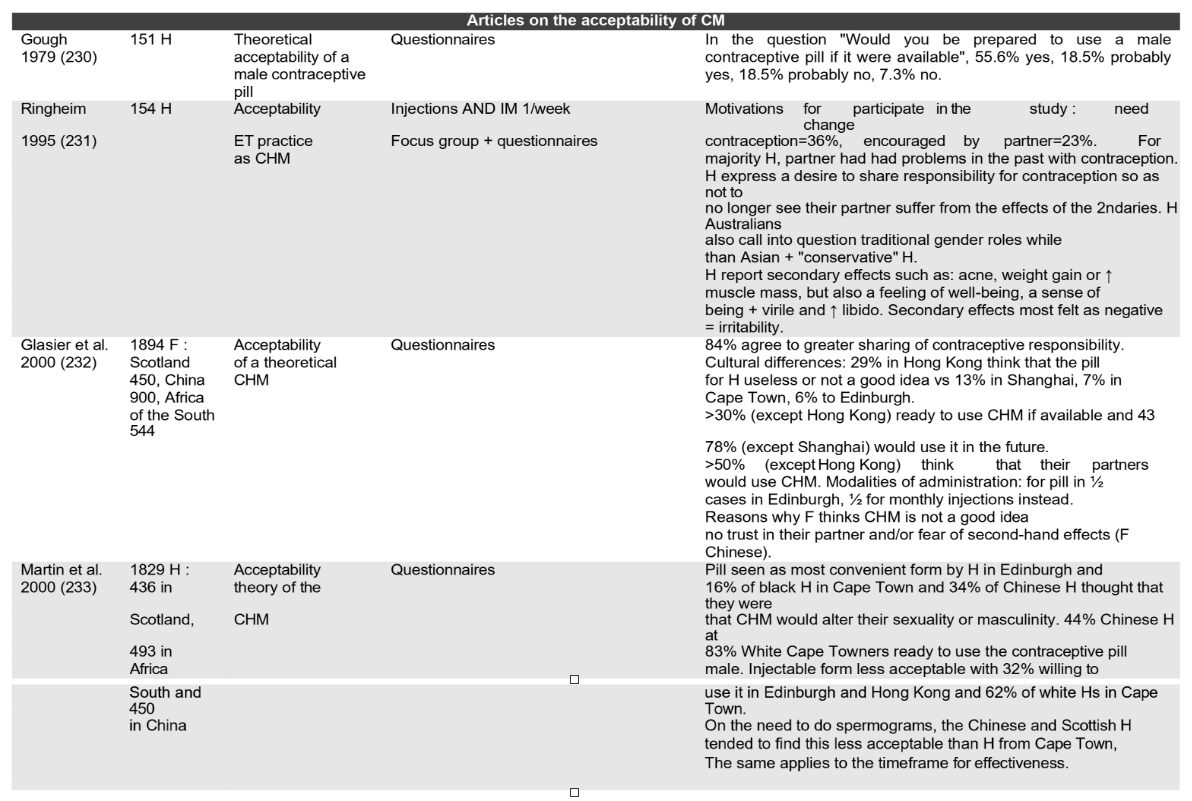
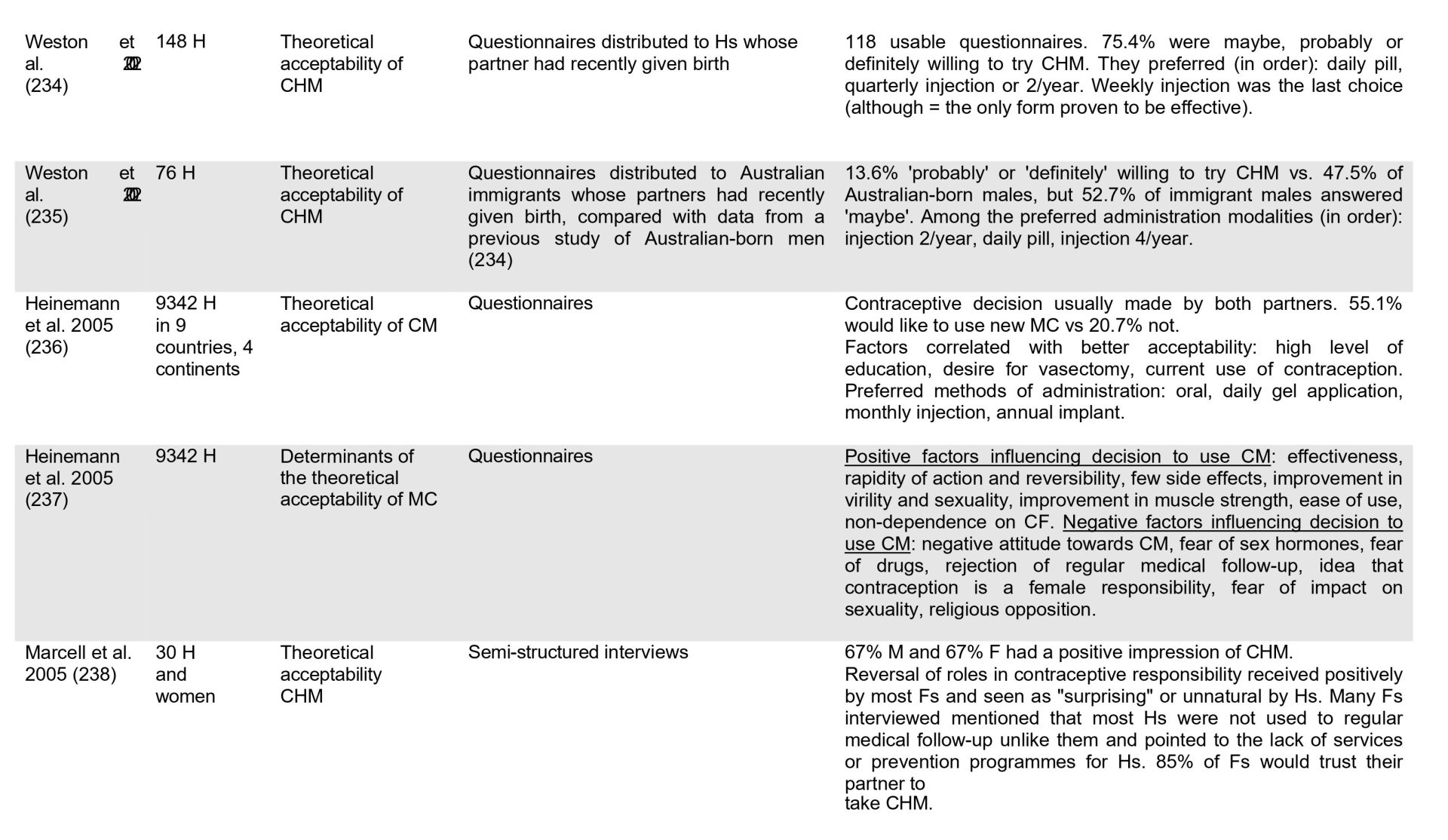
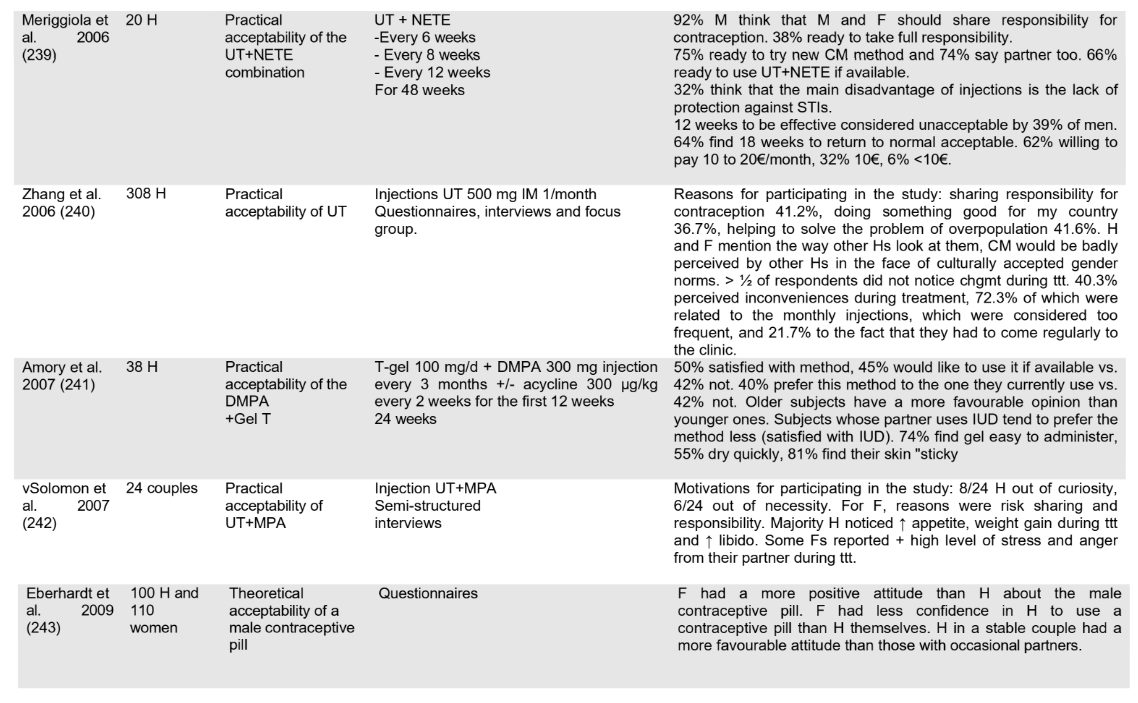
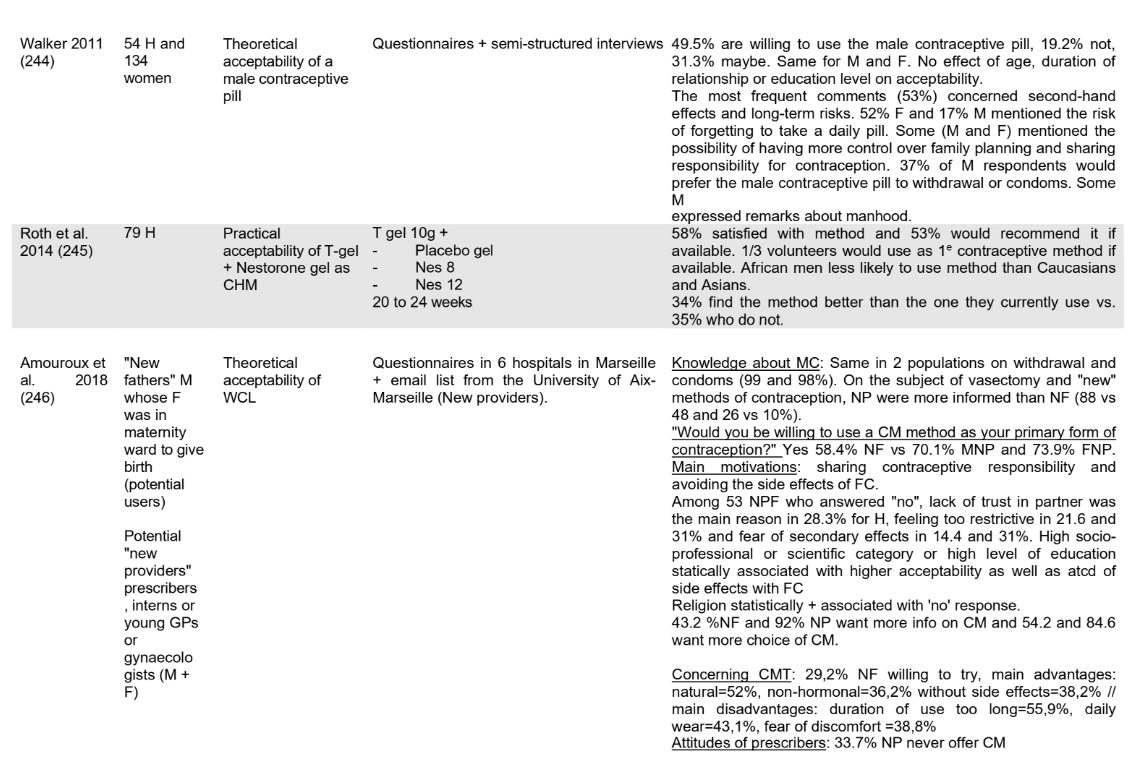
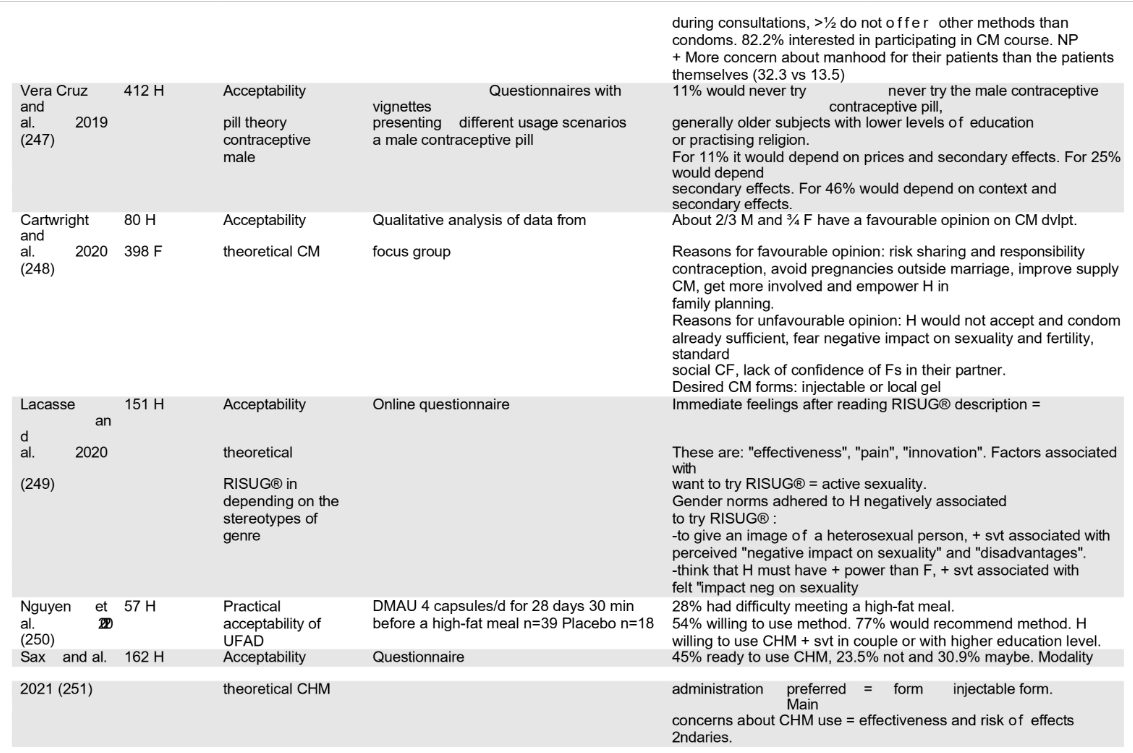
From 1979 to 2022, work shows increasing acceptability.
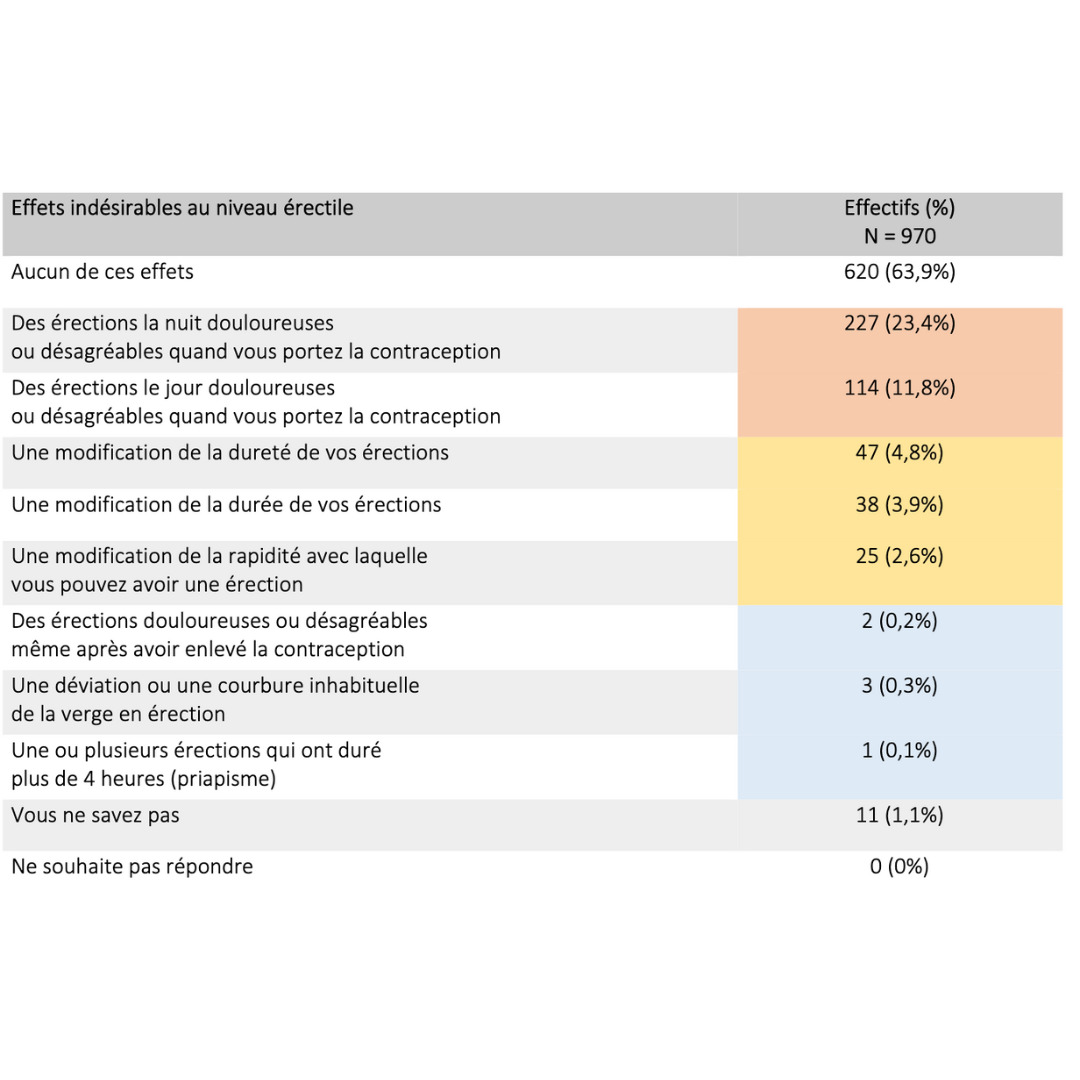
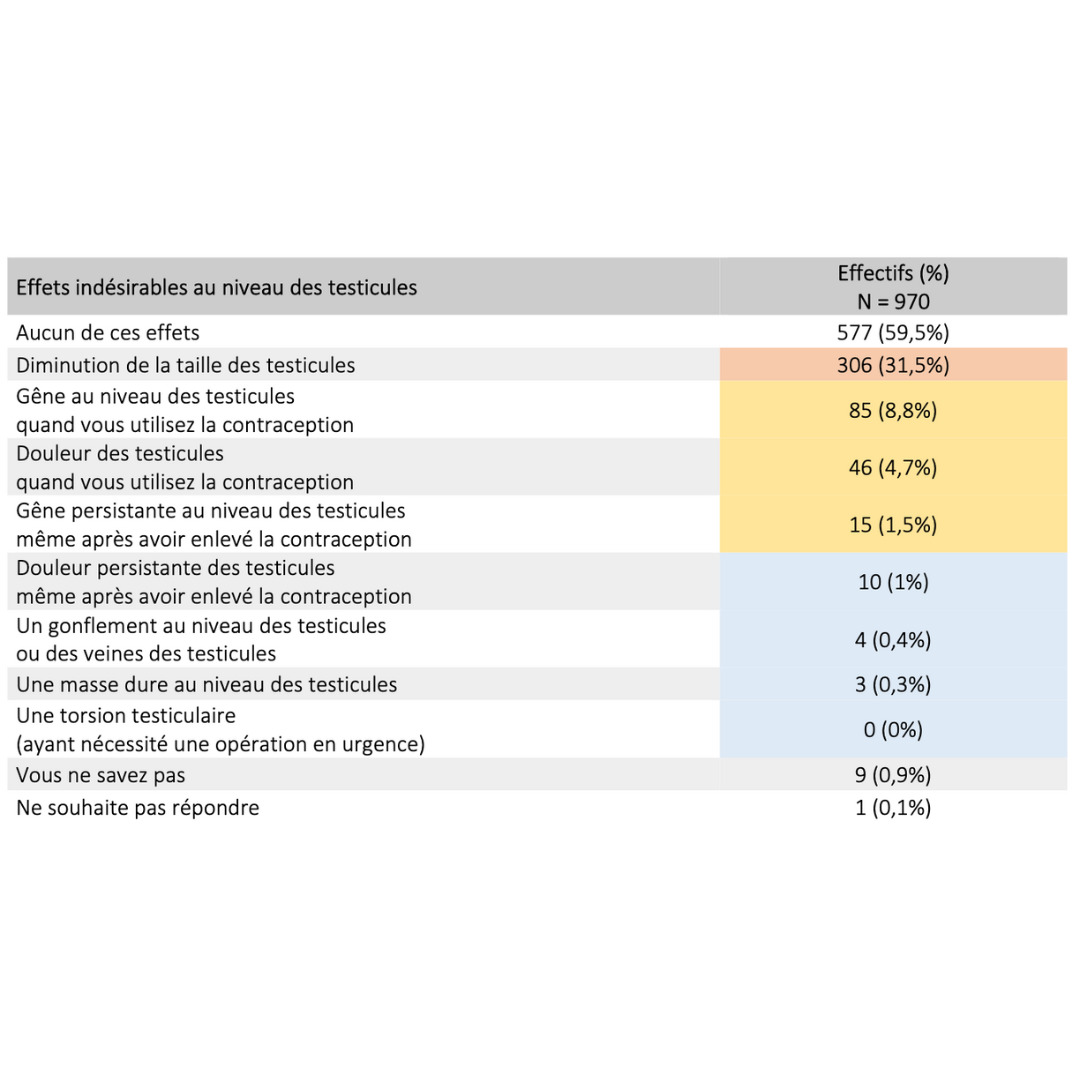
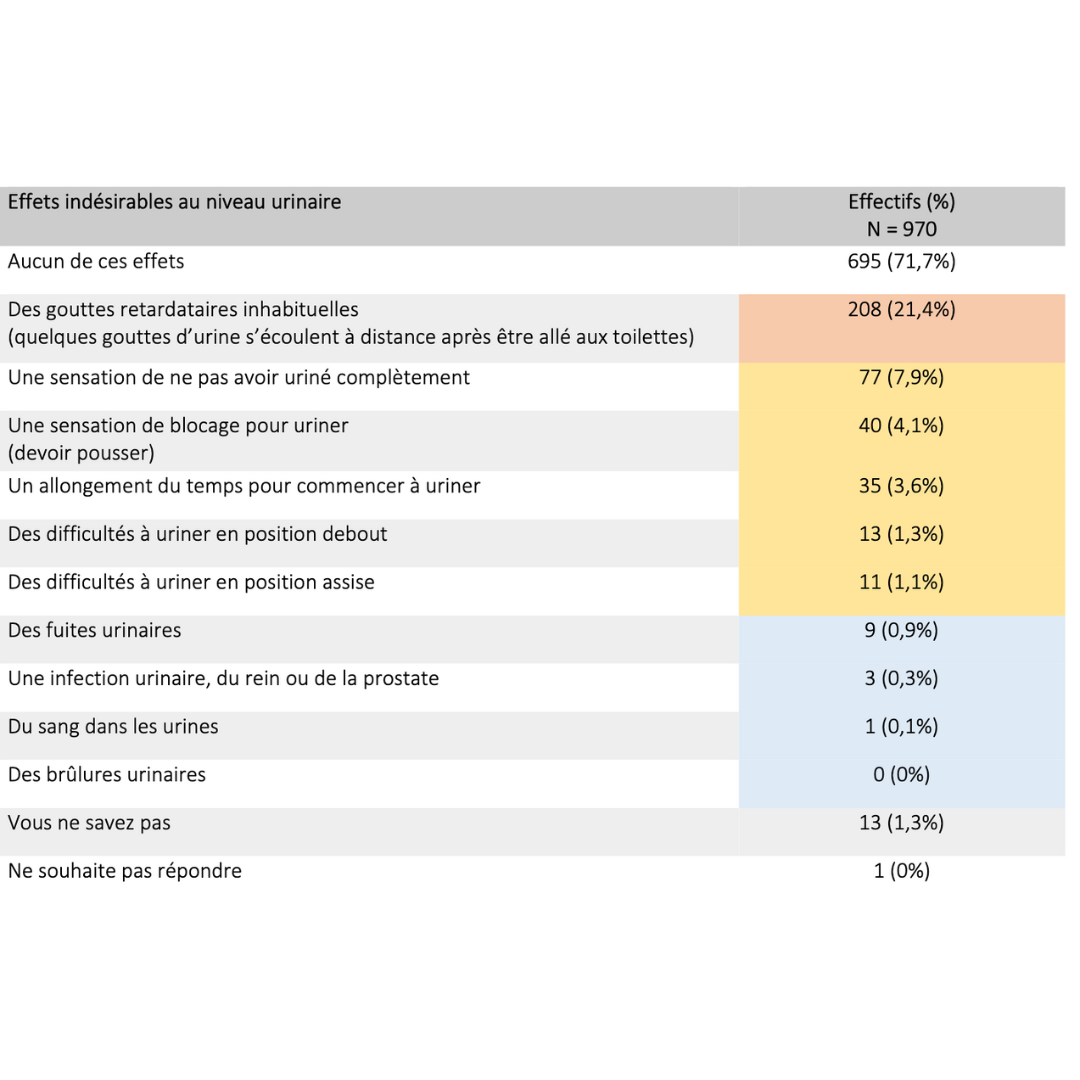
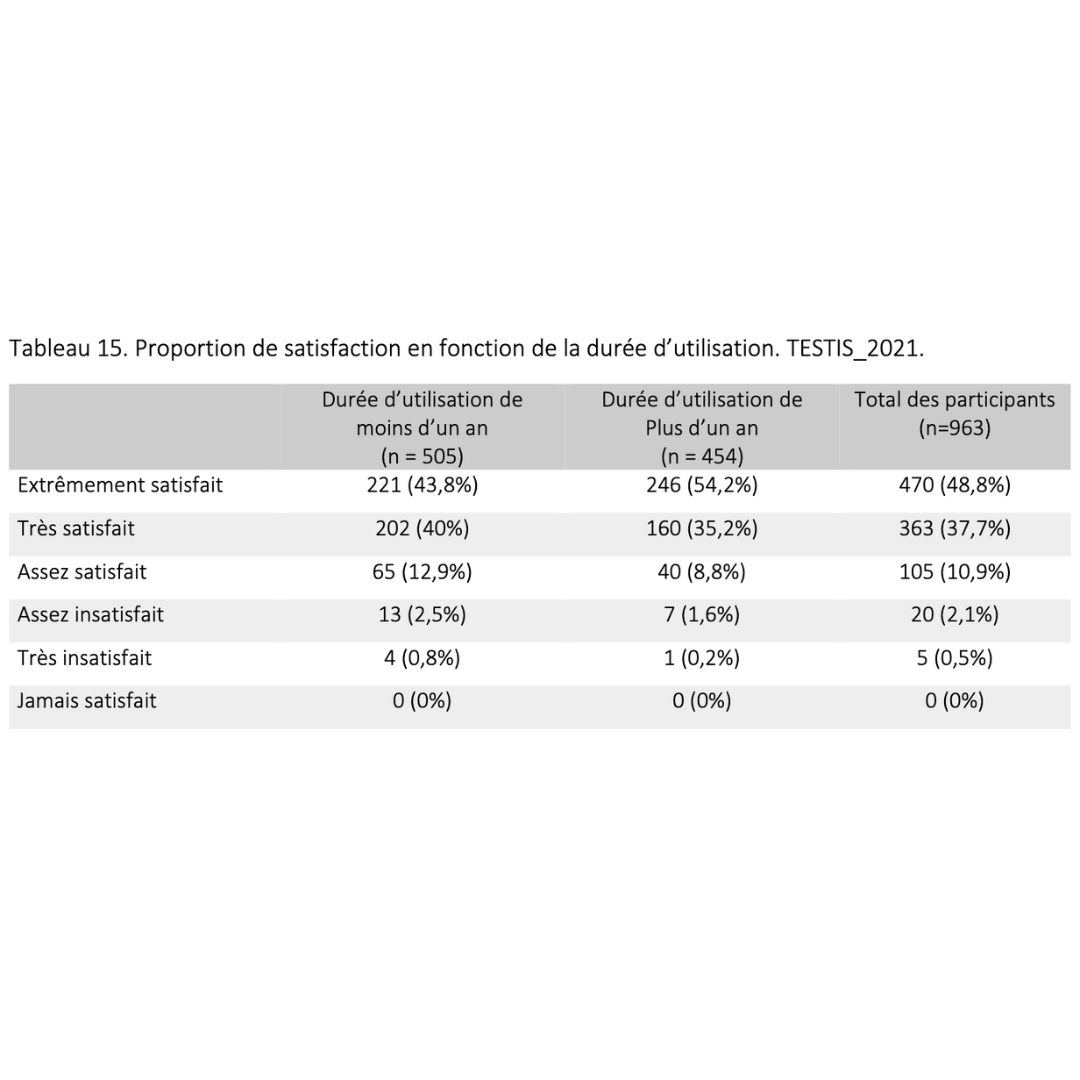
Side effects & benefits
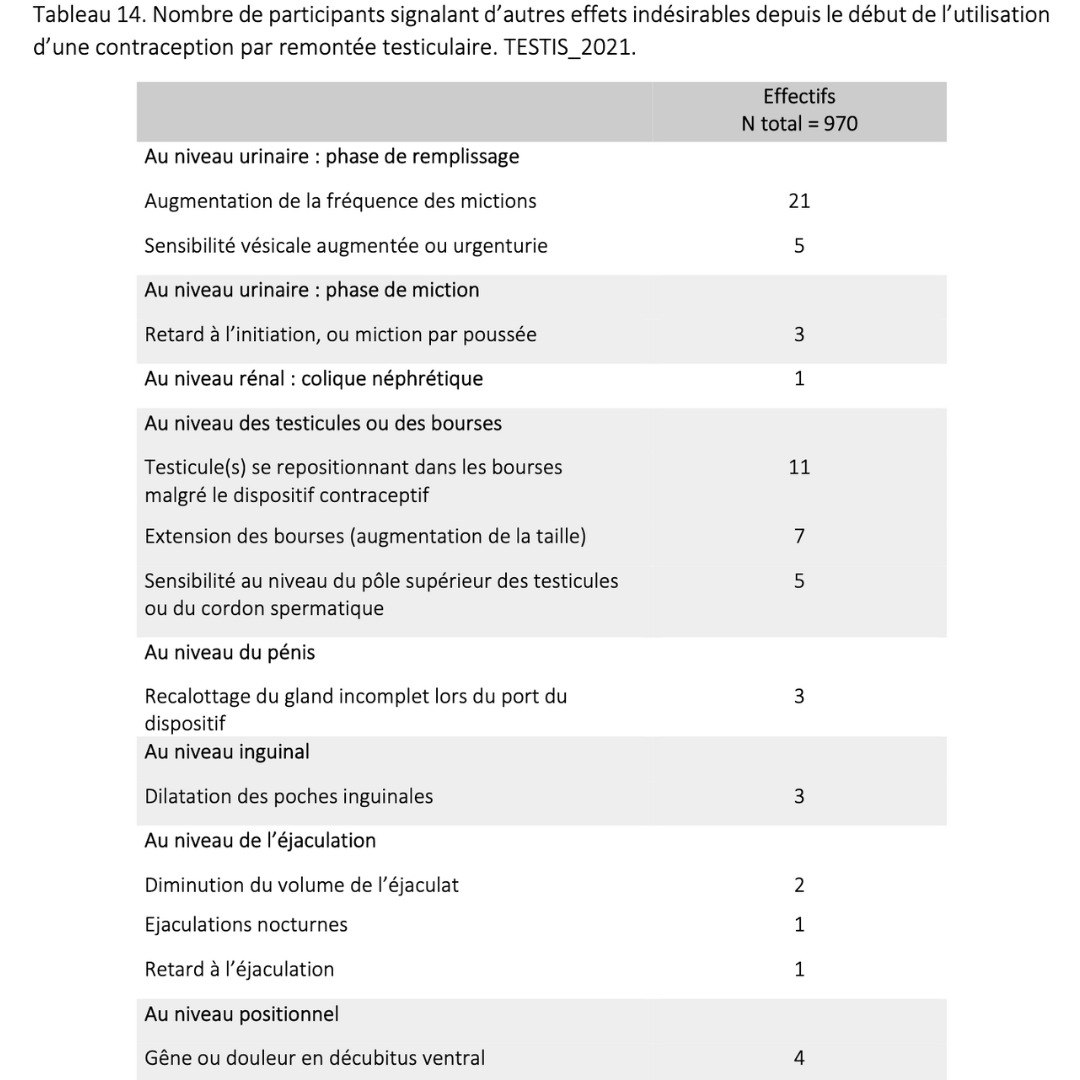
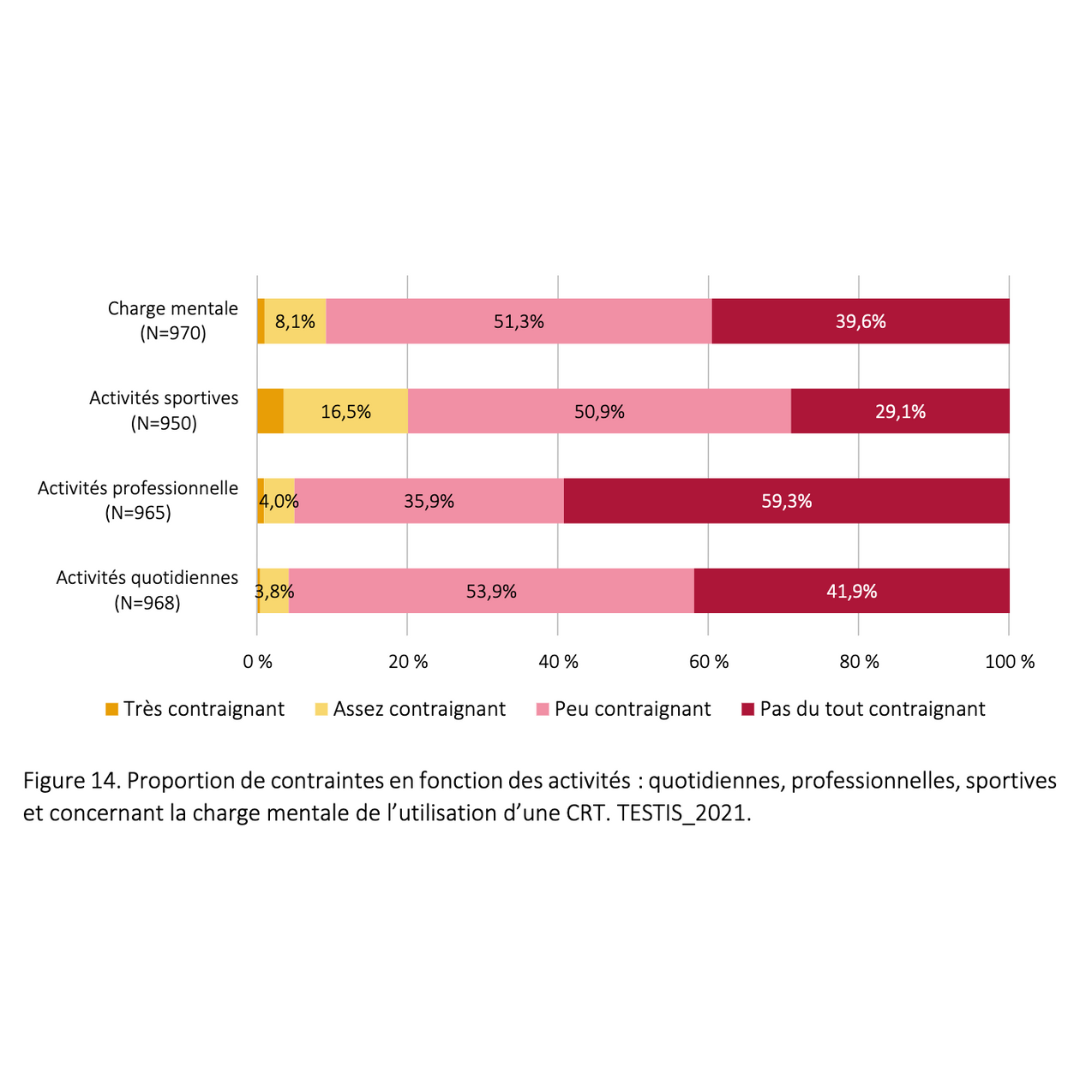
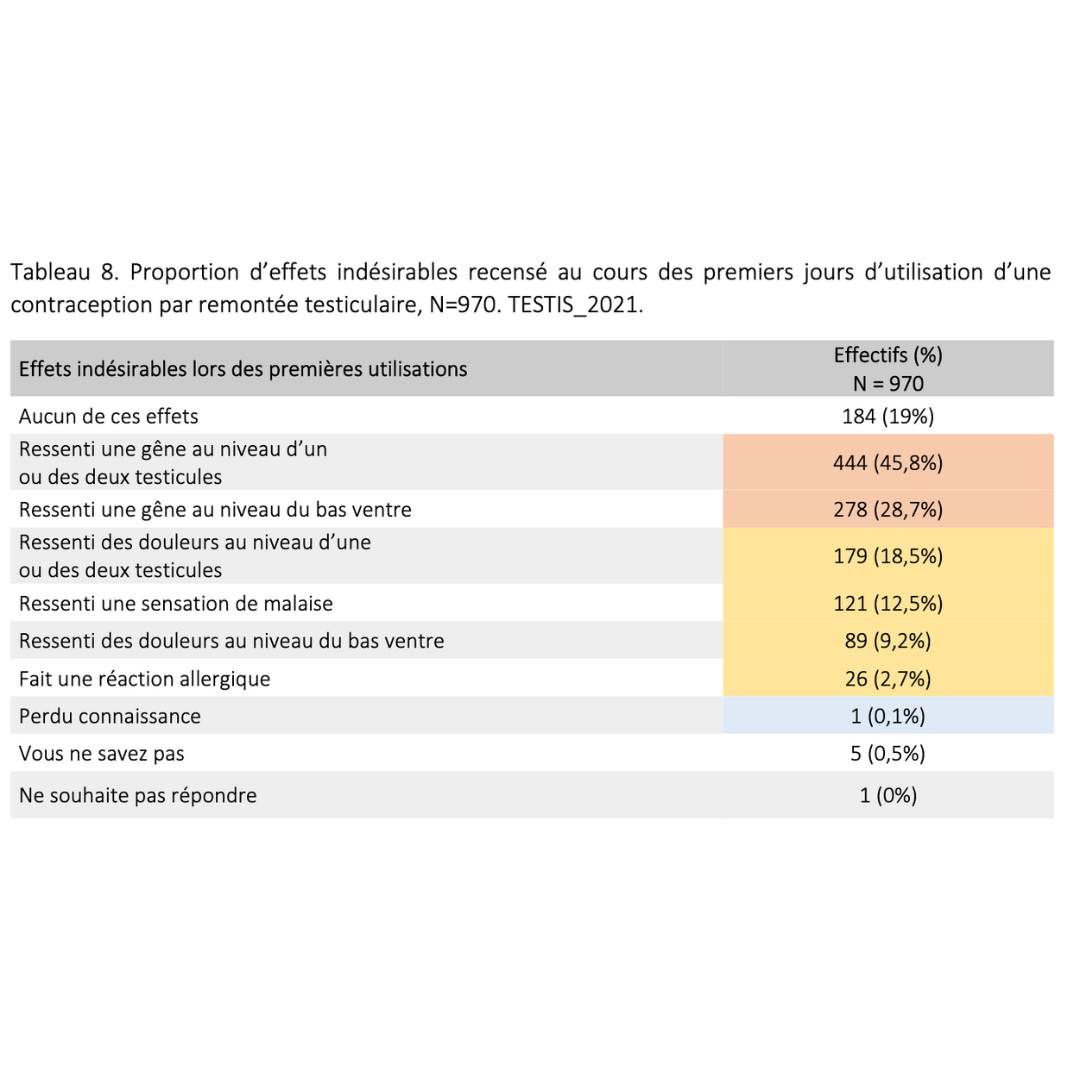
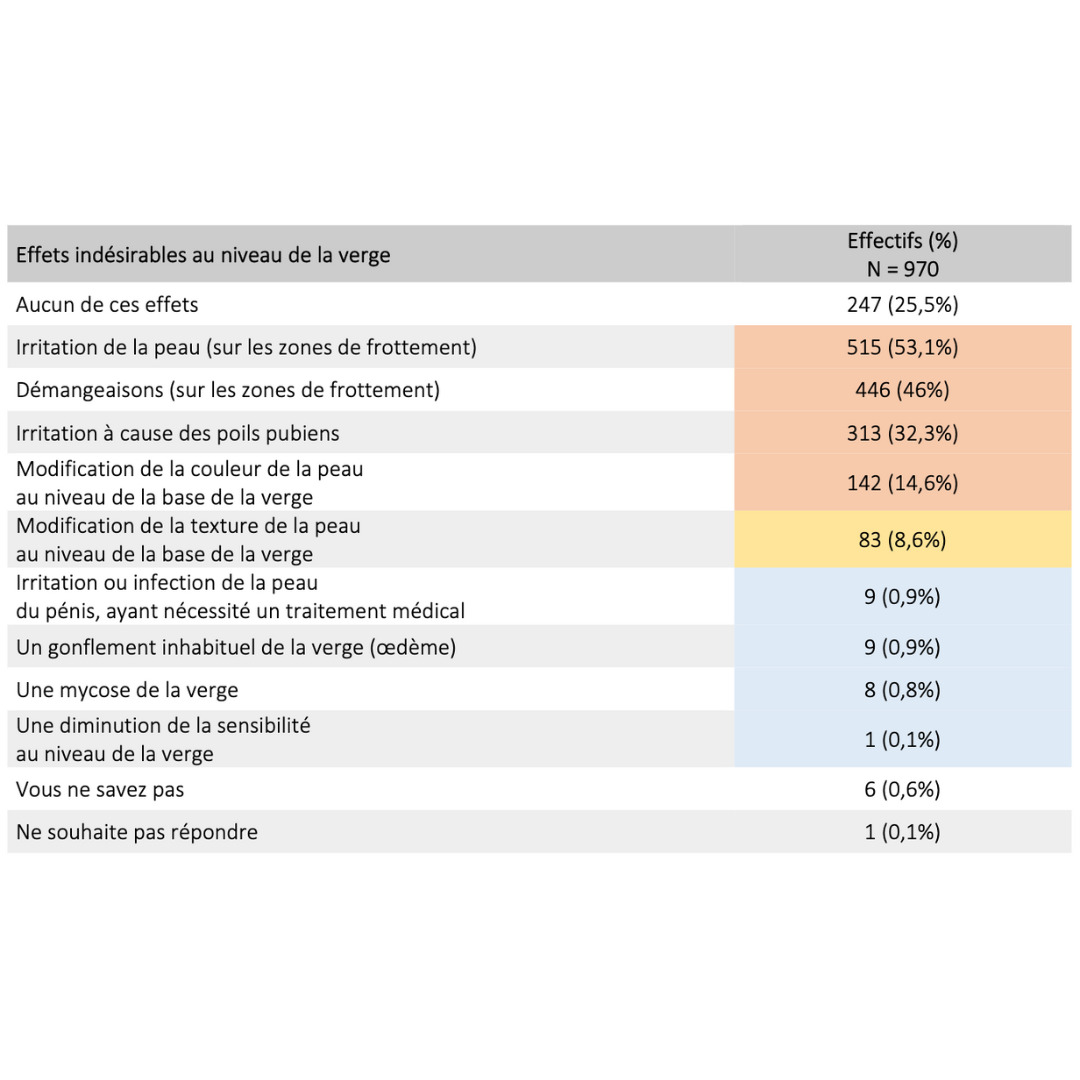
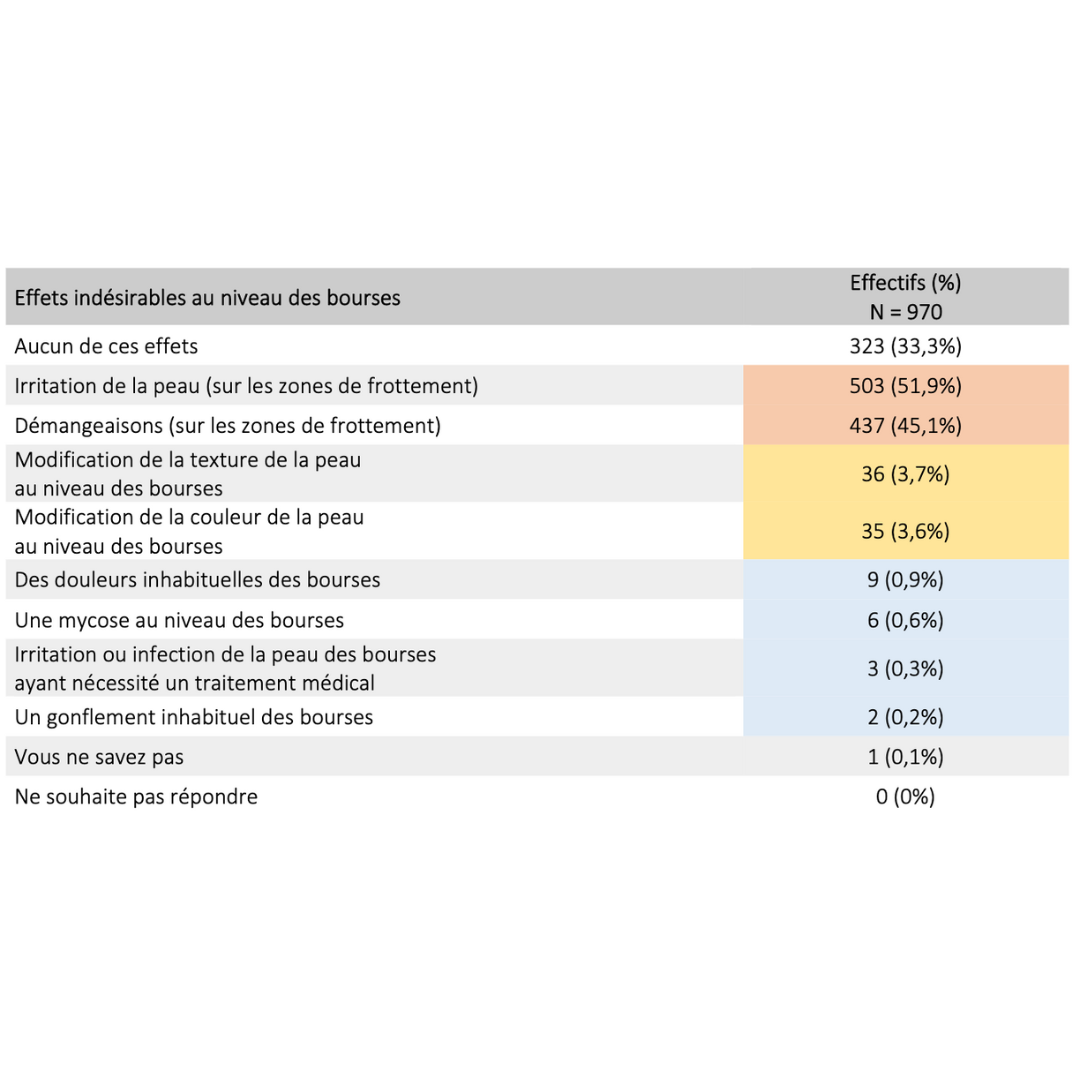
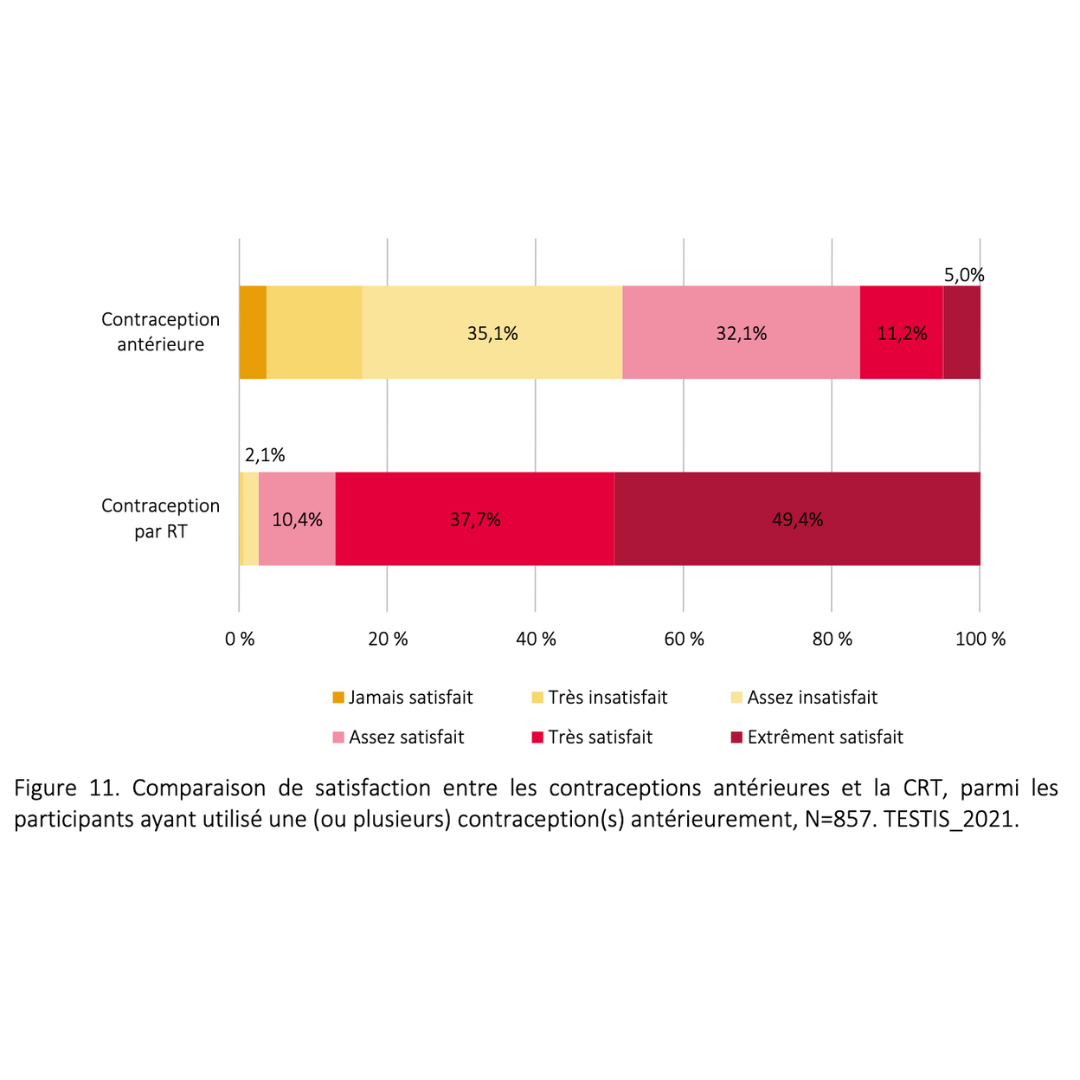
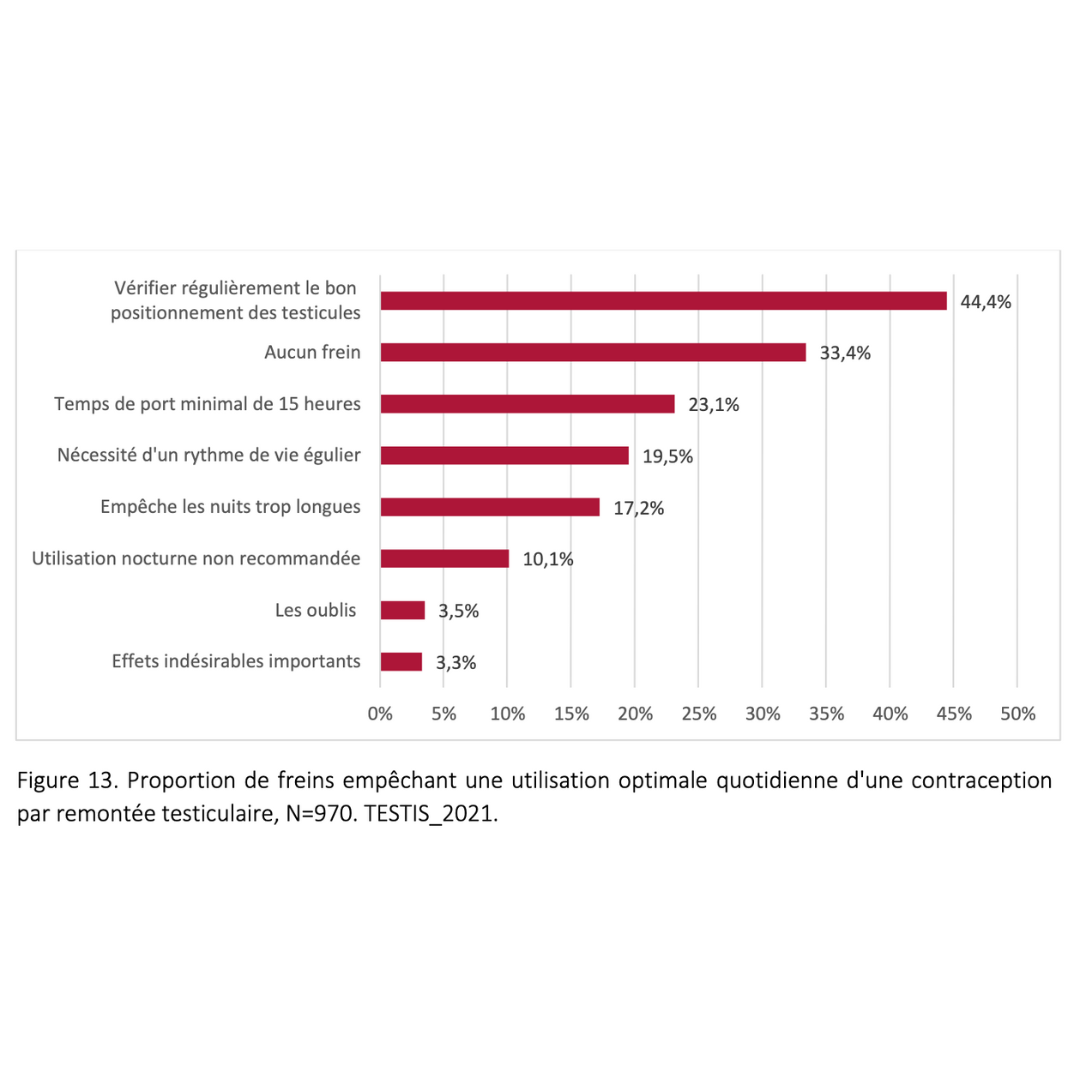
Data extracted from a retrospective cohort of over 900 users who had been in practice for more than 6 consecutive months.
2023 Guidarelli Cross-sectional study on testicular ascent contraception methods: safety, acceptability, effectiveness
Reassuring recommendations on grey areas:
Risk of malformation in pregnancy
2022 - Member of the Centre de Référence sur les Agents Tératogènes (Crat) and of the Académie Nationale de Médecine
"The risk is highly theoretical, since the development possibilities for eggs carrying chromosomal missegregation are very limited.
"The risk is highly theoretical, since the development possibilities for eggs carrying chromosomal missegregation are very limited. There is no need to propose termination of pregnancy, as the risks are very limited. The only thing to consider is prenatal diagnosis specifically designed to detect chromosomal number anomalies (blood marker tests with an early ultrasound scan at 12 weeks' gestation), and further prenatal diagnostics if the result is positive or doubtful."
Risk of testicular cancer
Protocols if you forget to wear your ring
Daily exposure to body heat is crucial. Mistakes happen, and here are some guidelines based on user experience:
Training in testicular contraception

The range of training courses on male contraception has expanded in recent years:
It is now one ofANDPC's national priority orientations for CPD 2023-2025 (sheet no. 18).
Ressourcerie
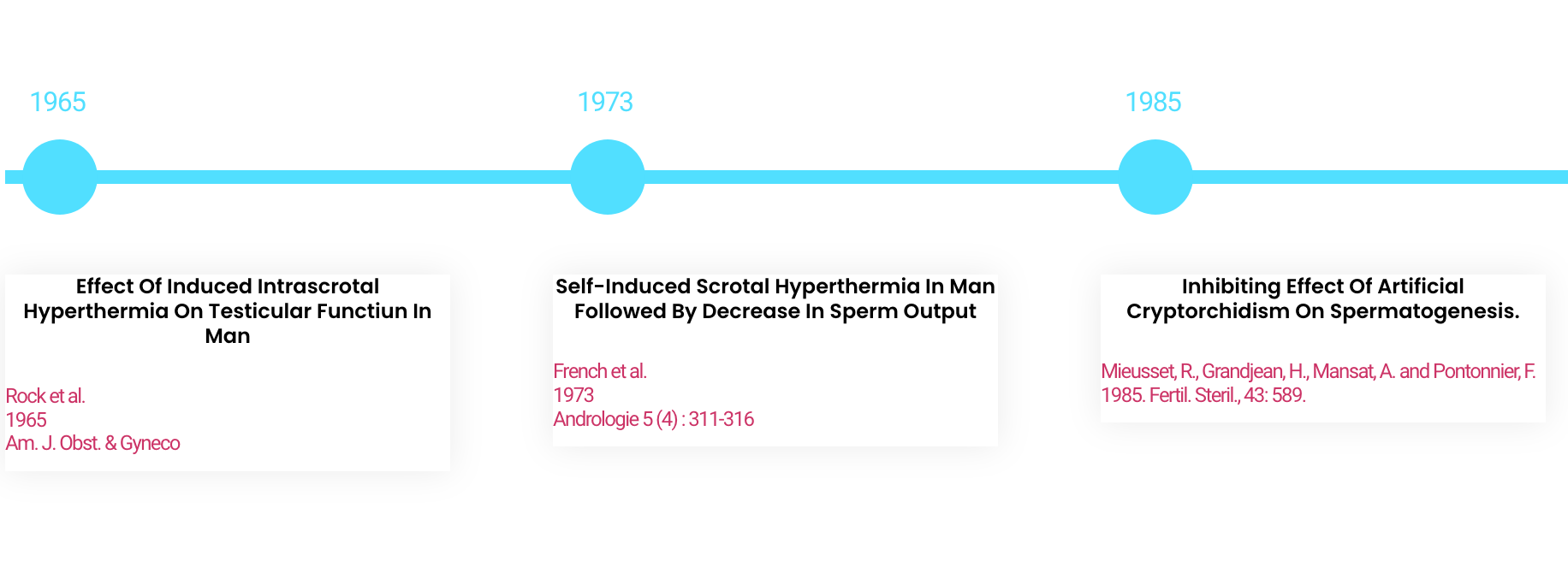
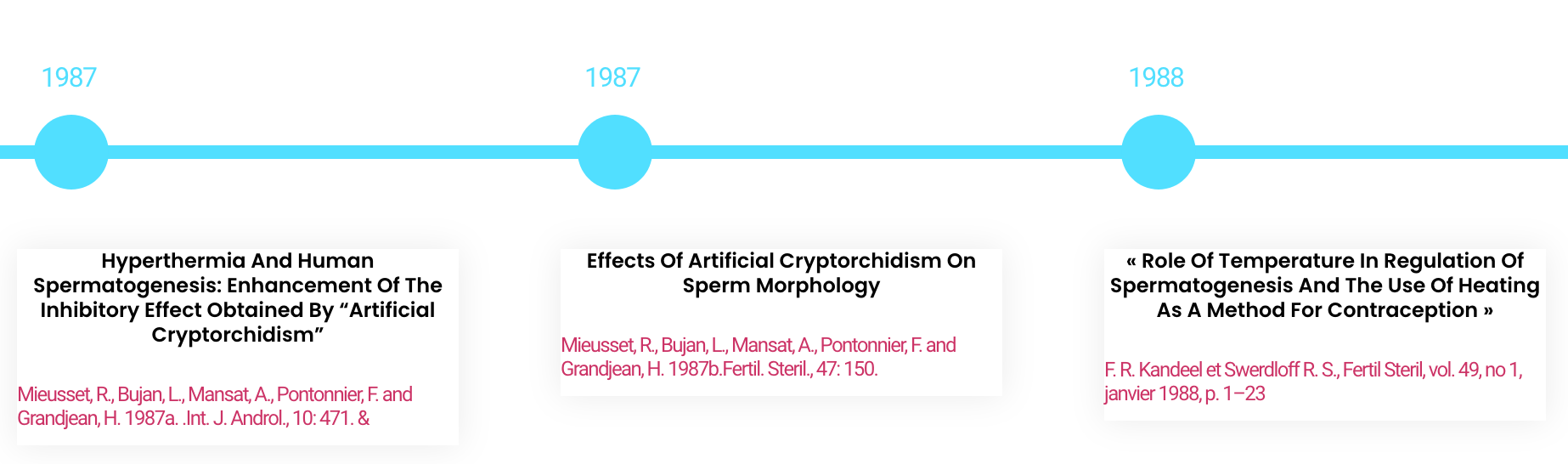
Scientific publications on male contraception
Clinical trials of the thermal method
Effect of induced intrascrotal hyperthermia on testicular functiun in man
Self-induced scrotal hyperthermia in man followed by decrease in sperm output
Inhibiting effect of artificial cryptorchidism on spermatogenesis.
Hyperthermia and human spermatogenesis: enhancement of the inhibitory effect obtained by "artificial cryptorchidism"
Effects of artificial cryptorchidism on sperm morphology
"Role of temperature in regulation of spermatogenesis and the use of heating as a method for contraception".
Heat Induced Inhibition of Spermatogenesis in Man.
Testicular suspension as a method of male contraception: technique and results
Contraceptive efficacy of polyester-induced azoospermia in normal men.
The potential of mild testicular heating as a safe, effective and reversible contraceptive method for men.
Polyester Sling in Indonesian Men 225 Cover Induces Oligozoospermia in Normal Indonesian Men
Proteomic analysis of testis biopsies in men treated with transient scrotal hyperthermia reveals the potential targets for contraceptive development"
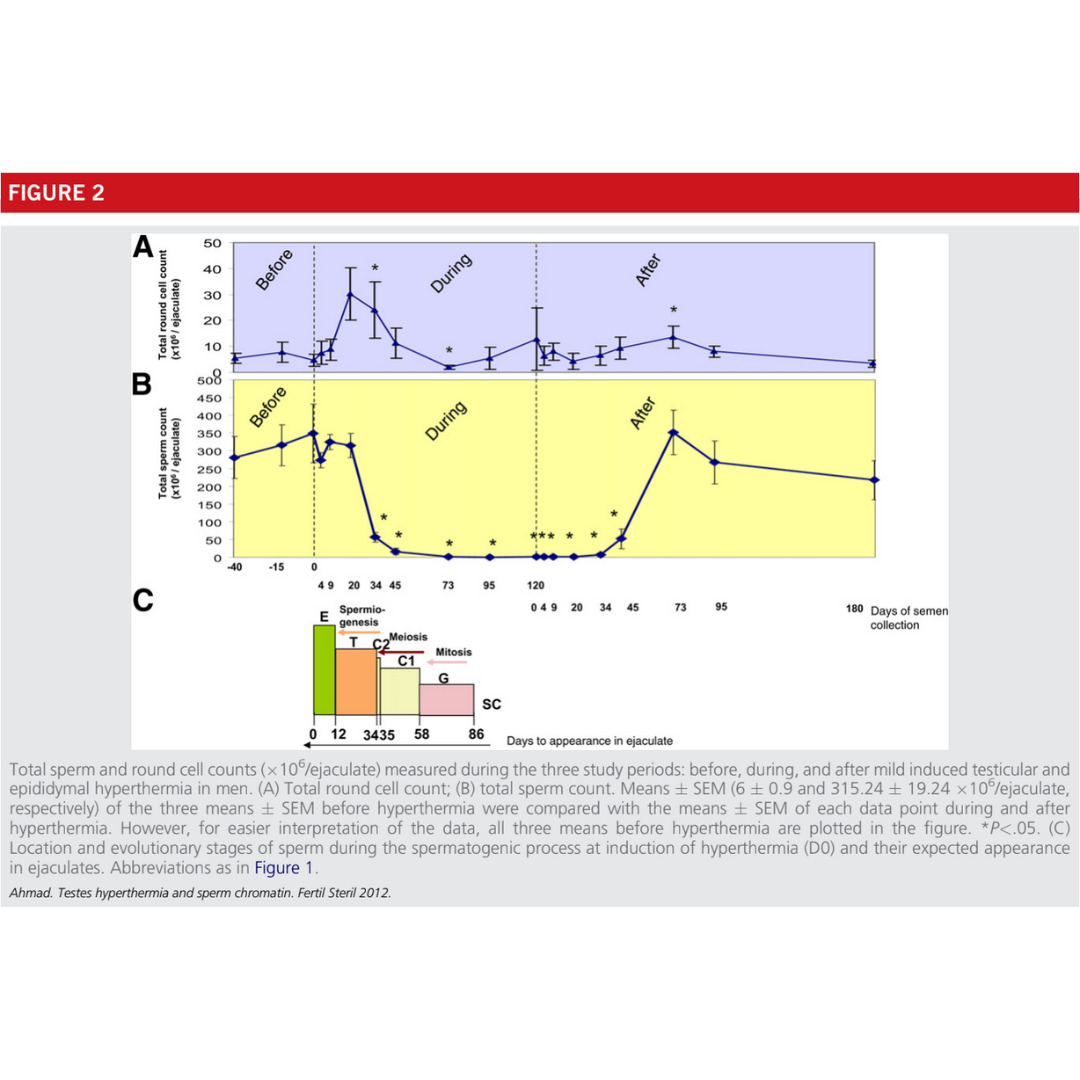
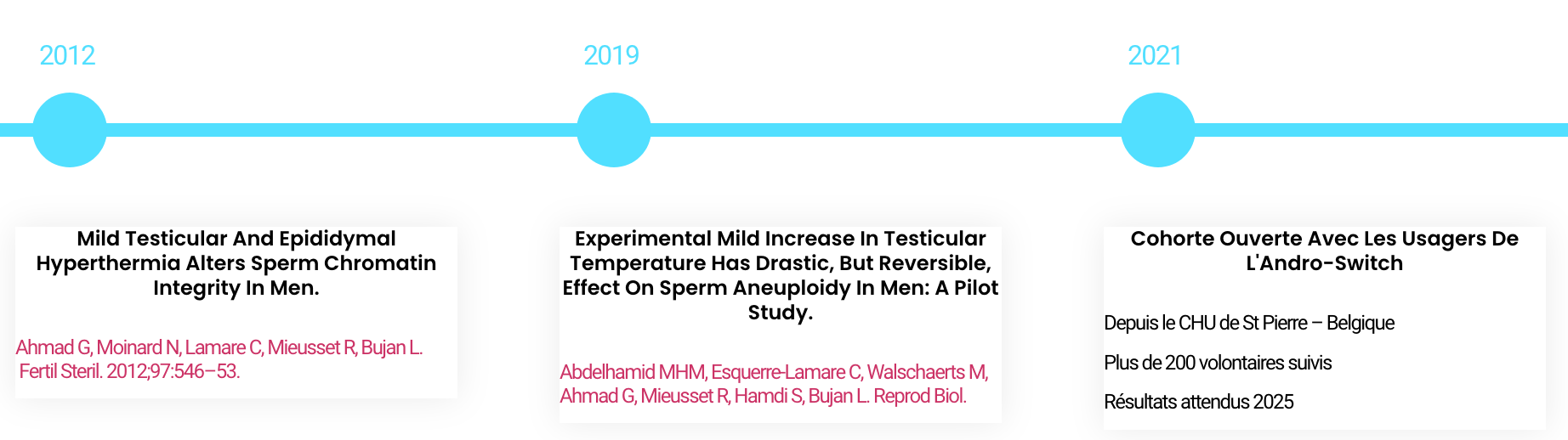
Mild testicular and epididymal hyperthermia alters sperm chromatin integrity in men.
Experimental mild increase in testicular temperature has drastic, but reversible, effect on sperm aneuploidy in men: A pilot study.
Open cohort with Andro-switch users
From St Pierre University Hospital - Belgium
More than 200 volunteers monitored
Expected results 2025
Acceptability of male thermal contraception among 900 users
Summary of Research 2017 - 2023

Clinical study on thermal testicular contraception
From HUG Geneva - Switzerland
Over 40 volunteers monitored
Expected results 2025
Clinical safety trial for the certification of the Andro-switch
To come, contact the cooperative